Maternal & Child Health
Addressing Disparities and Promoting Health Equity in Latino Communities
What is Latino Maternal and Child Health?
Latino maternal and child health focuses on the overall well-being of pregnant women, new mothers, and their children within the Latino community.
Hispanic women in the United States had the highest fertility rates from 2020 to 2022, averaging 63.3 births per 1,000 women aged 15-44 (March of Dimes Perinatal Data Center, 2024).
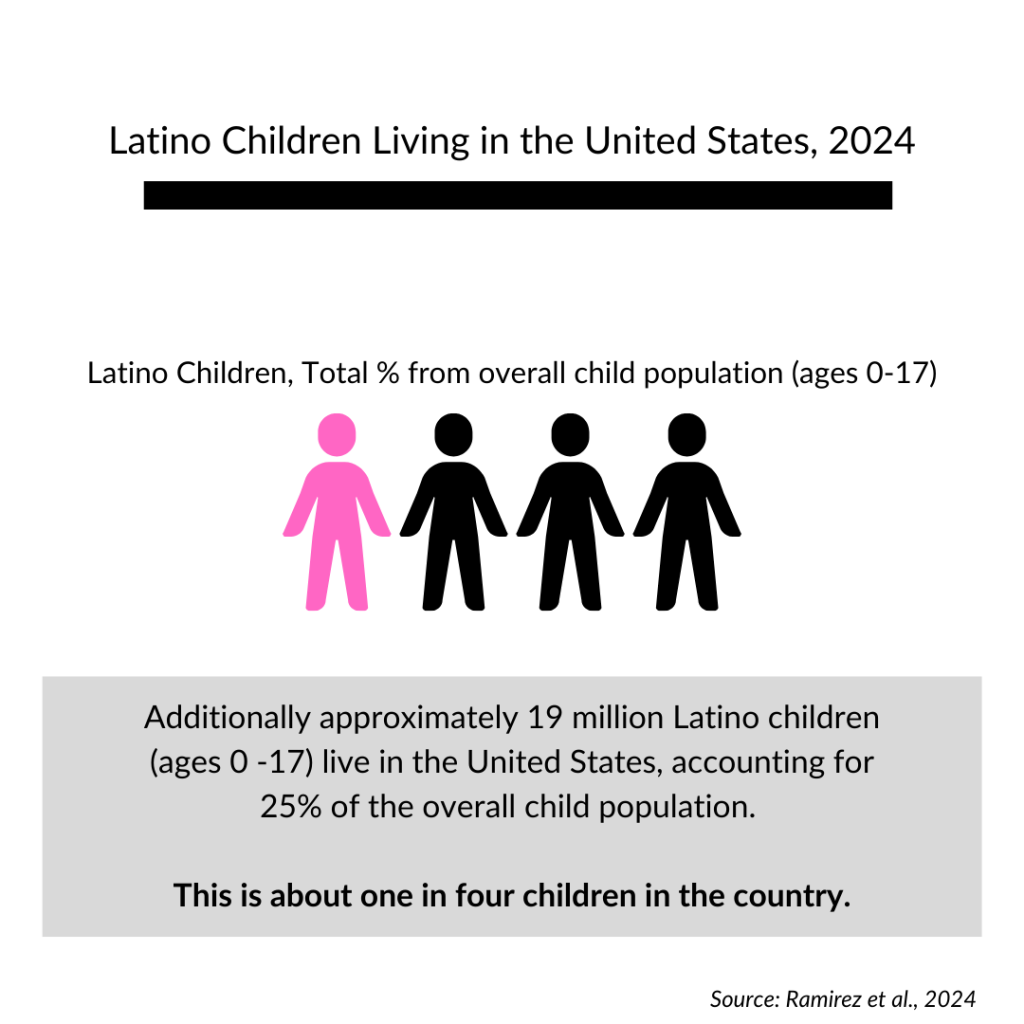
Additionally approximately 19 million Latino children (ages 0 -17) live in the United States, accounting for 25% of the overall child population. This is about one in four children in the country (Ramirez et al., 2024).
Key concerns include access to quality prenatal care, birth outcomes, infant mortality rates, and the general health of Latino children. Historically, the Latino community has encountered institutional impediments to healthcare access, language challenges, and economic disparities, all of which have contributed to inadequate child and maternal health outcomes.
High-Level Challenges:
Limited Access to Healthcare: Latino families face barriers to accessing adequate prenatal, maternity, and pediatric care due to language barriers, lack of insurance, and a shortage of medical practitioners (Fryer et al., 2021).
High Maternal Mortality Rates: Latina mothers have disproportionately high maternal death rates, which are typically caused by limited access to quality and affordable healthcare throughout pregnancy and delivery (The Commonwealth Fund, 2024a).
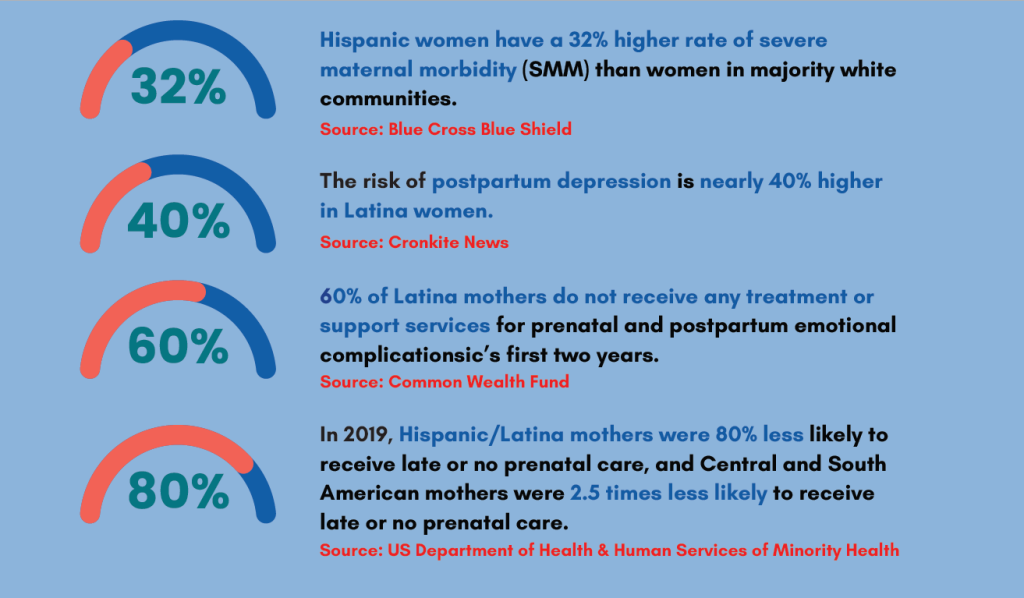
Mental Health Barriers for Mothers: High rates of prenatal depression and inadequate access to mental health care place additional burden on Latina mothers, negatively impacting both maternal and child well-being (Policy Center For Maternal Mental Health, 2023).
Infant Health Disparities: Latino infants have higher mortality rates and are more likely to have low birth weight due to insufficient prenatal care and socioeconomic disadvantages (Office of Minority Health, 2024).
Food Insecurity and Childhood Obesity: Due to a lack of inexpensive, healthy meal options, Latino children experience higher rates of food insecurity, which is frequently linked to childhood obesity. (Salud America, 2023)
Why This Issue Is Important to Latinos
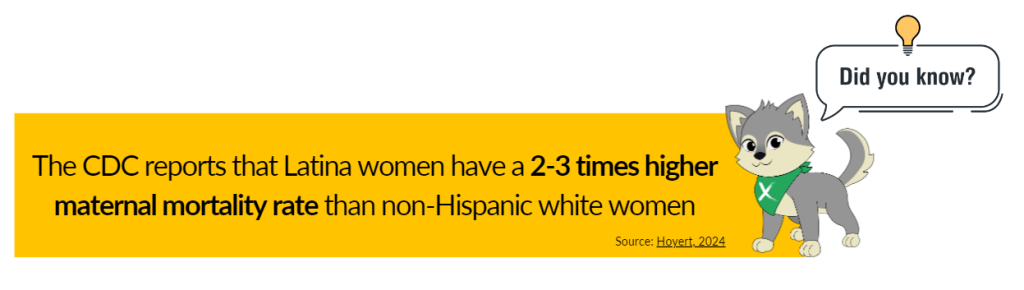
Latino families face disproportionate health challenges, including higher rates of maternal death, preterm births, and low birthweight. The CDC reports that Latina women have a 2-3 times higher maternal mortality rate than non-Hispanic white women (Hoyert, 2024).
Economic barriers, a lack of access to culturally appropriate care, and discrimination exacerbate these health inequities. These disparities have far-reaching societal consequences, including the financial strain on families and a lack of early childhood development support.
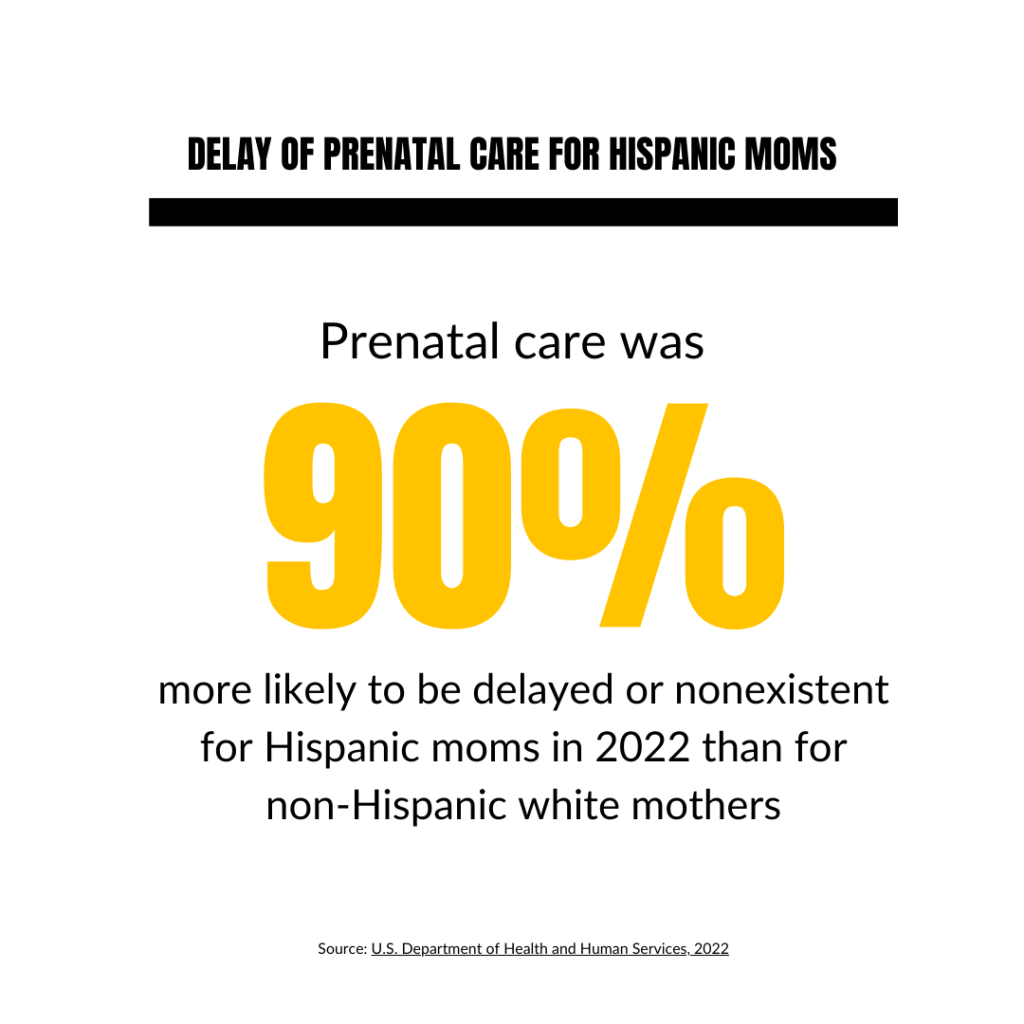
Prenatal Care Access: Prenatal care was 90% more likely to be delayed or nonexistent for Hispanic moms in 2022 than for non-Hispanic white mothers (U.S. Department of Health and Human Services, 2022). Accessibility to prenatal care is critical for monitoring both the health of mom and baby.
However, lack of coverage and linguistic difficulties prevent many Latina women from receiving adequate prenatal care. As a result, individuals are more likely to experience pregnancy difficulties, leading to poor delivery outcomes.
Maternal Mortality: Due to financial constraints and a lack of culturally appropriate treatment, Latina women have maternal death rates that are two to three times higher than those of non-Hispanic white women (Centers for Disease Control and Prevention, 2022).
This disparity emphasizes the need for systematic changes in the availability of safe, affordable medical care as well as culturally competent treatment in order to reduce unnecessary fatalities during pregnancy and delivery.
Mental Health in Mothers: Throughout the perinatal period, the prevalence of depression (moderate to severe) in Latina women ranges from 12 to 59%, while the general population’s prevalence is between 10 and 15% (Harris & Santos, 2020).
Latina mothers frequently face barriers to mental health services, and they have higher rates of prenatal depression. Addressing mental health as a component of maternity care is crucial to ensure maternal well-being and positive child outcomes.

Infant Health: In 2022, infant mortality rates for Hispanic and Latino subgroups ranged from 3.9 to 6.3 per 1,000 live births. Puerto Ricans had a 40% higher infant mortality rate than non-Hispanic whites (U.S. Department of Health and Human Services, 2022).
Maintaining the health of infants is essential for lowering death rates and laying a solid basis for long-term wellbeing. Physical and developmental success is more likely to be attained by healthy babies, which can have a big impact on their quality of life along with future contributions to their communities and families.
Childhood Nutrition: In 2022, food insecurity affected 20.8% of Latino households, while it only affected 9.3% of white households (Despres, 2023). Food insecurity along with childhood obesity are more common among Latino children due to inadequate availability of healthy meals. Addressing nutrition within early childhood is critical for avoiding chronic health problems and supporting long-term health.
Data: Key Statistics
- According to the Centers for Disease Control and Prevention (CDC), U.S. maternal mortality worsened during the pandemic, particularly for Latinas. In 2020, the U.S. saw 23.8 maternal deaths per 100,000 live births, an 18.4% increase from 2019. For Hispanic women, this rate surged by 44%, highlighting the severe impact of the pandemic on Latina mothers. (Centers for Disease Control and Prevention, 2022).
- 20.8% of Latino households experienced food insecurity in 2022 (vs. 9.3% for White households). This is a higher food insecurity rate than 2021 (15%). (Despres, 2023).
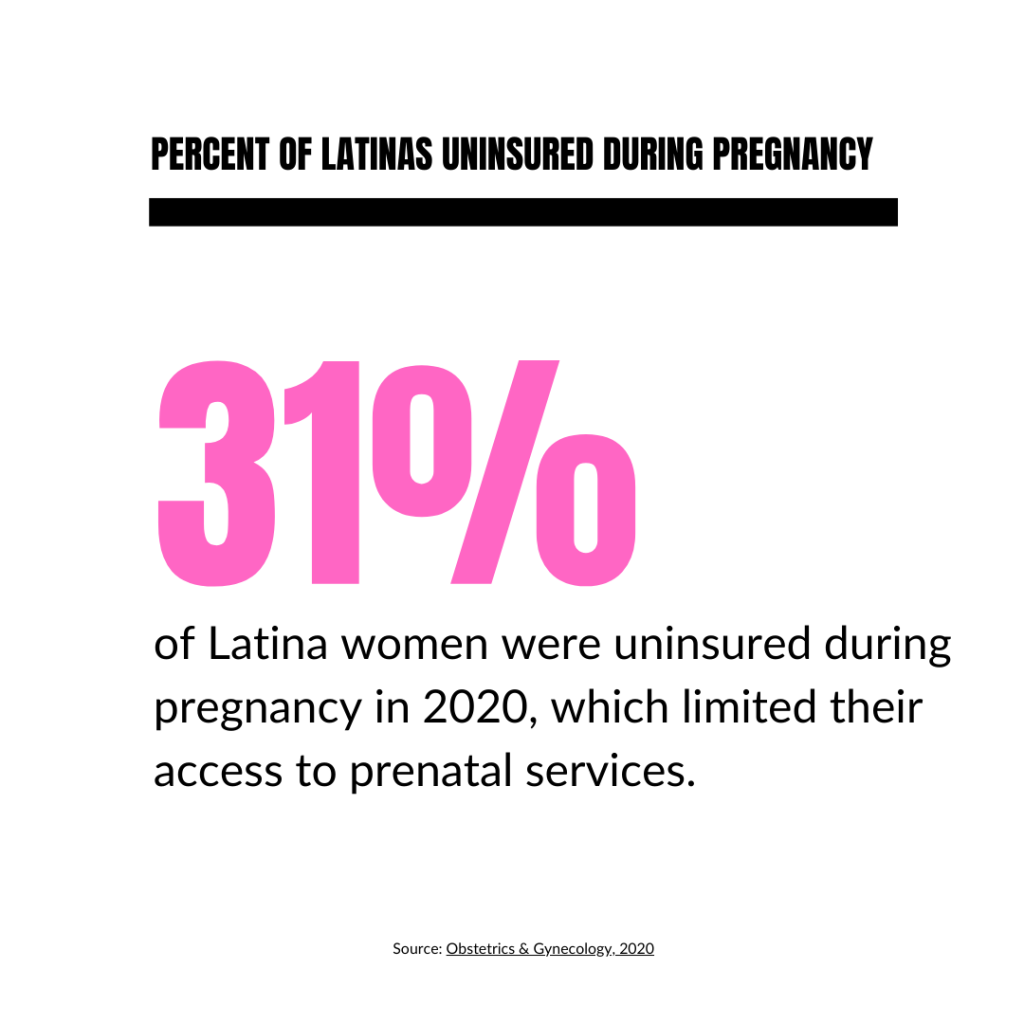
- Approximately 31% of Latina women were uninsured during pregnancy in 2020, which limited their access to prenatal services. (Obstetrics & Gynecology, 2020)
- In 2022, Hispanic mothers were 90% more likely to receive late or no prenatal care as non-Hispanic white mothers (U.S. Department of Health and Human Services, 2022).
- Puerto Rican infants were 2 times as likely to die from causes related to maternal complications of pregnancy than non-Hispanic white infants in 2022 (U.S. Department of Health and Human Services, 2022).
- Prevalence rates of depression (mild to severe) in Latina mothers range from 12 to 59% in the perinatal period, compared to 10–15% in the general population. Moreover, lack of accessible, affordable, and culturally competent mental health care for Latina mothers has been well-documented (Harris & Santos, 2020).
- Low-income Hispanic women on Medicaid have a 28% higher rate of complications. (Coombs, 2023).
Programming, Policies & Recommendations
Current Policies
Note: These are existing policies we’ve compiled that are related to Maternal and Child Health.
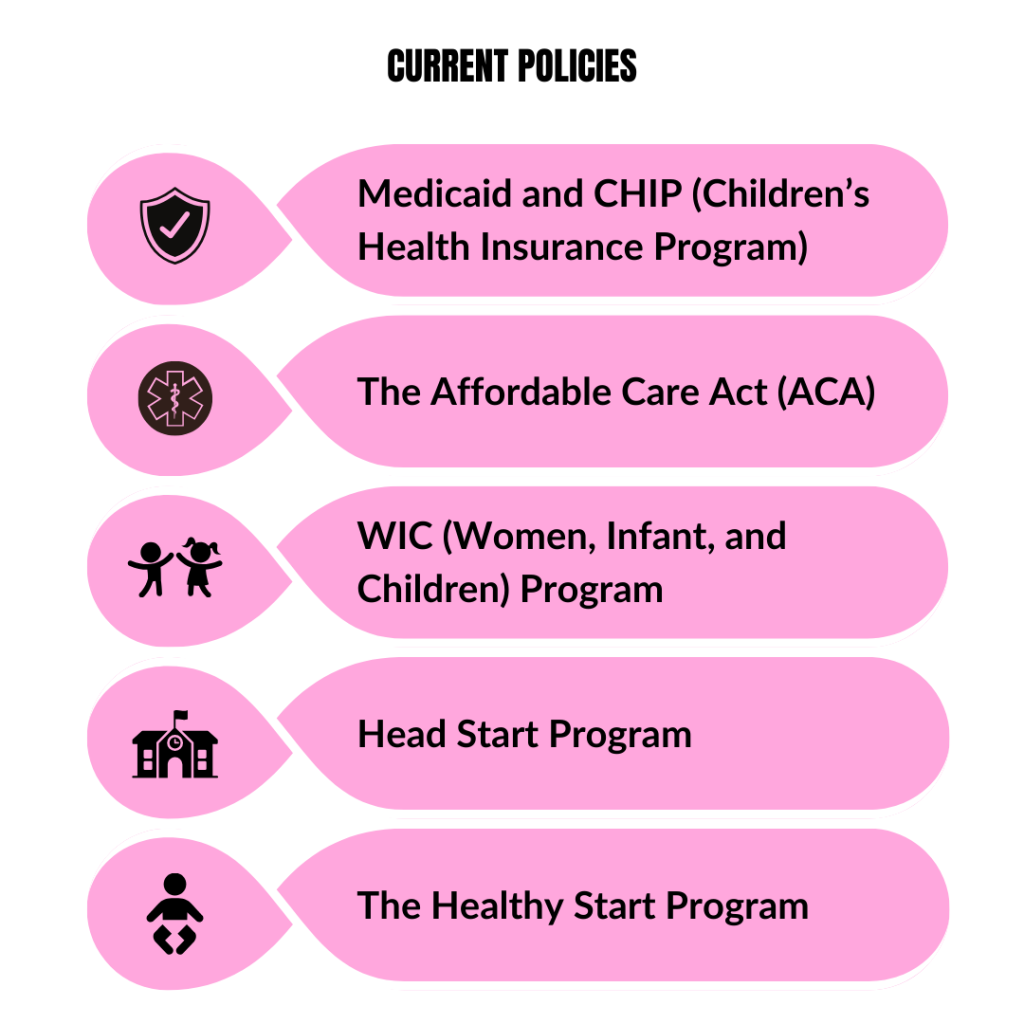
Medicaid and CHIP (Children’s Health Insurance Program)
1. What Are Medicaid and CHIP?
- Medicaid: Established in 1965, Medicaid is a joint federal-state program that provides health coverage to low-income individuals, including children, pregnant women, elderly adults, and people with disabilities. Each state administers its Medicaid program within federal guidelines, leading to variations in coverage and services across states (Medicaid.gov).
- CHIP: Created in 1997, the Children’s Health Insurance Program (CHIP) offers health coverage to children in families with incomes too high for Medicaid but too low to afford private insurance. Like Medicaid, CHIP is jointly funded by federal and state governments, leading to differences in benefits across states (Medicaid.gov).
2. Impact
- Reduction in Uninsured Rates: CHIP has significantly decreased the number of uninsured children in the U.S., reducing the uninsured rate among children by half since its inception (MACPAC.gov).
- Financial Protection for Families: Medicaid and CHIP help reduce medical debt and financial hardship for low-income families by covering a significant portion of healthcare costs (KFF.org).
- Improved Health Outcomes: Access to Medicaid and CHIP is linked to better overall health, earlier disease detection, and increased preventive care visits, especially for children (NIH.gov).
3. Why Are Medicaid and CHIP Helpful?
- Comprehensive Health Coverage: These programs provide extensive benefits, including doctor visits, hospital care, preventive services, immunizations, and prescriptions, ensuring low-income families have access to essential healthcare (Medicaid.gov).
- Increased Preventive Care Access: Children enrolled in Medicaid and CHIP are more likely to receive preventive services, which contribute to early disease detection and improved long-term health (KFF.org).
- Greater Coverage for Vulnerable Populations: Medicaid expansion under the Affordable Care Act (ACA) extended coverage to millions of low-income adults who were previously uninsured (Commonwealth Fund).
4. Challenges
- State-by-State Variation in Benefits: Medicaid benefits vary across states, creating disparities in coverage and quality of care depending on location (KFF.org).
- Complex Eligibility and Enrollment Processes: Medicaid and CHIP require extensive documentation and frequent redetermination, making it difficult for individuals to maintain continuous coverage (GAO.gov).
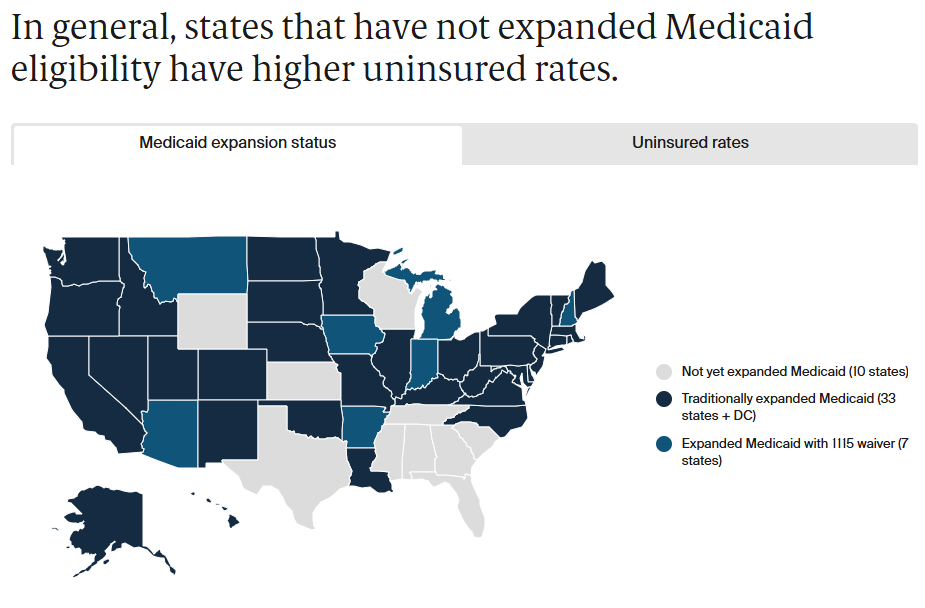
- Coverage Gaps in Non-Expansion States: Some low-income individuals remain uninsured in states that have not expanded Medicaid under the ACA, leaving millions without affordable health coverage (KFF.org).(Drake et al., 2024).
- Low Provider Participation: Many healthcare providers do not accept Medicaid patients due to low reimbursement rates, limiting access to care for enrollees (NIH.gov).
The Affordable Care Act (ACA)
1. What Is ACA?
- The Affordable Care Act (ACA), enacted in 2010, is a comprehensive healthcare reform law aimed at expanding health insurance coverage, reducing healthcare costs, and improving the healthcare delivery system in the United States. HHS
2. Impact
- Increased Health Insurance Coverage: Since its implementation, the ACA has significantly increased health insurance coverage across the United States. As of early 2024, more than 45 million people were enrolled in Marketplace or Medicaid expansion coverage under provisions of the ACA, marking the highest total on record. PubMed Central+2aspe.hhs.gov+2aspe.hhs.gov+2
- Protection for Preexisting Conditions: Approximately 43 million Latinos with chronic health issues, such as high blood pressure, are now protected from insurance company discrimination based on preexisting conditions. UnidosUS
- Gender-Based Premium Protections: Nearly 20 million Latinas are protected from insurance company discrimination based on gender, preventing higher premiums solely because of their gender. UnidosUS
3. Why Is It Helpful?
- Enhanced Access to Preventive Services: The ACA mandates coverage for preventive services, including prenatal visits and screenings, at no additional cost, reducing health risks for mothers and infants.
- Support for Community Health Centers: Increased funding for Community Health Centers under the ACA has bolstered affordable, culturally competent care for Latino communities. PubMed Central
4. Challenges:
- State Expansion: Numerous low-income Latino families in the affected states were left without coverage because some states chose not to expand Medicaid under the Affordable Care Act (Lukens & Harker, 2024).
- Private Insurance Rates: Private insurance rates are still too expensive for certain Latino families, even with subsidies, especially for those who make just over the Medicaid poverty threshold (Betancourt, 2024).
- Enrollment Barriers: Some qualified Latino families may find it difficult to enroll in and navigate ACA health plans, particularly if they have inadequate digital literacy or English ability (Villagra et al., 2019).
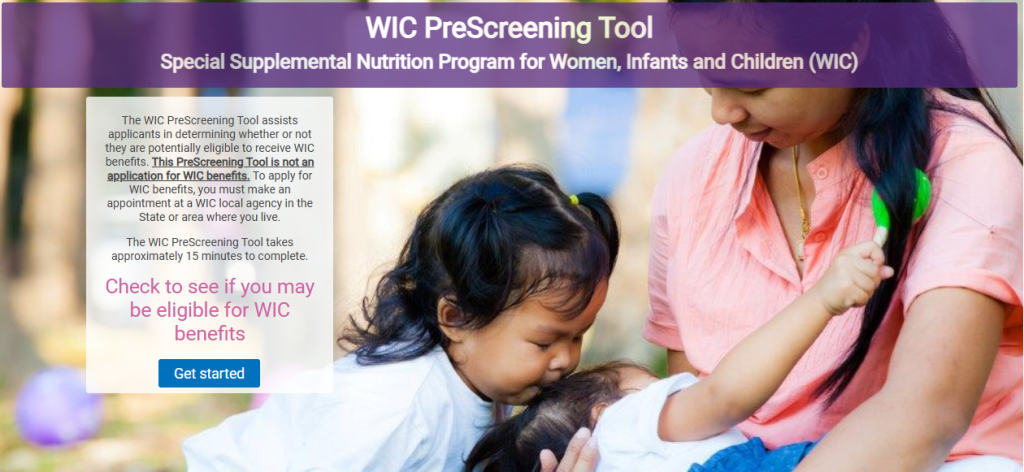
WIC (Women, Infant, and Children) Program
1. What Is It?
- The WIC program provides nutritional assistance, education, and healthcare referrals to low-income pregnant, breastfeeding, and postpartum women, as well as infants and children up to age five who are at nutritional risk. Food and Nutrition Service
2. Impact
- Improved Birth Outcomes: WIC participation is associated with longer pregnancies, fewer premature births, and lower incidence of low birth weight, contributing to improved birth outcomes. Center for Budget and Policy Priorities
- Enhanced Child Health: Children enrolled in WIC are more likely to receive regular preventive healthcare services, such as well-child check-ups and immunizations, leading to better health outcomes. publichealth.jhu.edu
- Cost Savings: Every dollar spent on WIC results in savings of up to $4.21 by reducing the risk of preterm births and associated medical costs. drexel.edu
3. Why Is It Helpful?
- Nutritional Support: WIC provides access to nutritious foods, promoting healthy diets among participants. Food and Nutrition Service
- According to studies, WIC membership improves food intake while also lowering low birth weight and infant death rates (Lin, 2022; Sonchak, 2016).
- Health Education: Participants receive nutrition education and breastfeeding support, empowering them to make informed health decisions.
- Healthcare Referrals: WIC offers referrals to healthcare and social services, facilitating comprehensive care for families. Center for Budget and Policy Priorities
4. Challenges
- Limited Reach: Despite its benefits, WIC reaches only about half of those eligible, indicating a gap in program participation. Center for Budget and Policy Priorities
- WIC serves 53 percent of all infants born in the United States (U.S. Department of Agriculture, 2024).
- Eligibility Restrictions: The program is limited to specific groups—pregnant women, infants, and young children—excluding other vulnerable populations who may also benefit from nutritional support.
- Access Barriers: Participants may face challenges such as stigma and limited access to WIC offices, particularly in rural areas. Code for America
- Funding Constraints: Inadequate funding could force states to put eligible new and expecting parents and young children on waiting lists for nutrition assistance, limiting the program’s effectiveness. Center for Budget and Policy Priorities
Head Start Program (HRSA)
1. What Is It?
- Established in 1965, the Head Start Program is a federally funded initiative in the United States designed to promote school readiness for children from low-income families. It provides comprehensive early childhood education, health, nutrition, and parent involvement services to children from birth to age five. https://acf.gov/ohs/about/head-start
2. Impact
- Support for Latino Children: Head Start’s emphasis on early childhood development and school readiness significantly benefits Latino children, who may face educational challenges due to socioeconomic and linguistic factors. The program helps bridge gaps in school preparedness. National Health Service Alliance
- Comprehensive Services: Head Start offers nutrition, mental health services, and health screenings, supporting the development of Latino children and educating parents about their children’s health needs.
- Cultural and Linguistic Responsiveness: Many Head Start programs employ bilingual staff and utilize culturally appropriate materials to create a welcoming environment for Latino families, fostering increased parental involvement. acf.hhs.gov
- Family Engagement: Head Start programs often involve families in events and activities, helping Latino families feel supported and connected to other parents and community resources.
3. Why Is It Helpful?
- Early Educational Intervention: By focusing on early childhood education, Head Start addresses educational disparities, preparing Latino children for academic success. American Community Forum
- Health and Nutrition Support: The program’s health and nutrition services ensure that children receive necessary medical attention and develop healthy eating habits, contributing to overall well-being. American Community Forum
- Parental Empowerment: Through active family engagement, Head Start empowers parents with knowledge and resources, enhancing their ability to support their children’s development. American Community Forum
4. Challenges
- Budget Constraints: Due to budget and capacity constraints, numerous eligible Latino families might not be able to enroll in Head Start programs, particularly in high-need areas (National Head Start Association, 2022).
- Limited Bilingual Support: The availability of bilingual support varies, and some programs might not have the resources to address the needs of families whose Spanish is the primary language, even though many programs offer it (U.S. Department of Health and Human Services, 2019).
- Accessibility and Barriers: Although Early Head Start is beneficial for expectant mothers and children under three, it is frequently less accessible than the regular Head Start program, which limits Latino moms’ access to prenatal care and infant care resources (CLASP, 2016).
The Healthy Start Program (HRSA)
What Is It?
- Established in 1991, the Healthy Start Program is a federal initiative aimed at reducing infant mortality rates and improving perinatal outcomes by providing comprehensive health and social services to high-risk pregnant women, infants, and their families in communities with high rates of infant mortality. mchb.hrsa.gov
2. Impact
- Reduction in Infant Mortality and Adverse Birth Outcomes: The initiative has contributed to reductions in infant mortality, low birth weight, and preterm deliveries in high-risk communities by offering services such as prenatal care, nutrition counseling, and parental education. Maternal and Child Health Bureau
- Culturally Tailored Interventions: The Healthy Start program customizes interventions to meet the specific cultural and socioeconomic needs of communities, leading to increased participation and program effectiveness. Maternal and Child Health Bureau
- Improved Access to Healthcare Services: The program ensures that underserved communities have access to essential healthcare services and resources, reducing barriers for families and mothers in need. hrsa.gov
3. Why Is It Helpful?
- Comprehensive Support: Healthy Start provides a range of services, including prenatal and postpartum care, health education, and support services, addressing various factors that contribute to infant mortality and poor maternal health outcomes. https://mchb.hrsa.gov/programs-impact/healthy-start
- Community Engagement: By involving community members and tailoring services to local needs, Healthy Start fosters trust and encourages active participation, enhancing the program’s impact. policylink.org
4. Challenges
- Limited Long-Term Support: Once participants age out of the program, there may be challenges in maintaining positive outcomes due to limited long-term support for mothers and children. floridahealth.gov
- Resource Limitations: Healthy Start programs often operate with limited resources, which can restrict their capacity to reach all eligible families and provide comprehensive services. Government Accountability Office
- Variability in Service Quality: The availability and quality of services can vary by location, leading to inconsistent outcomes across different communities. link.springer.com
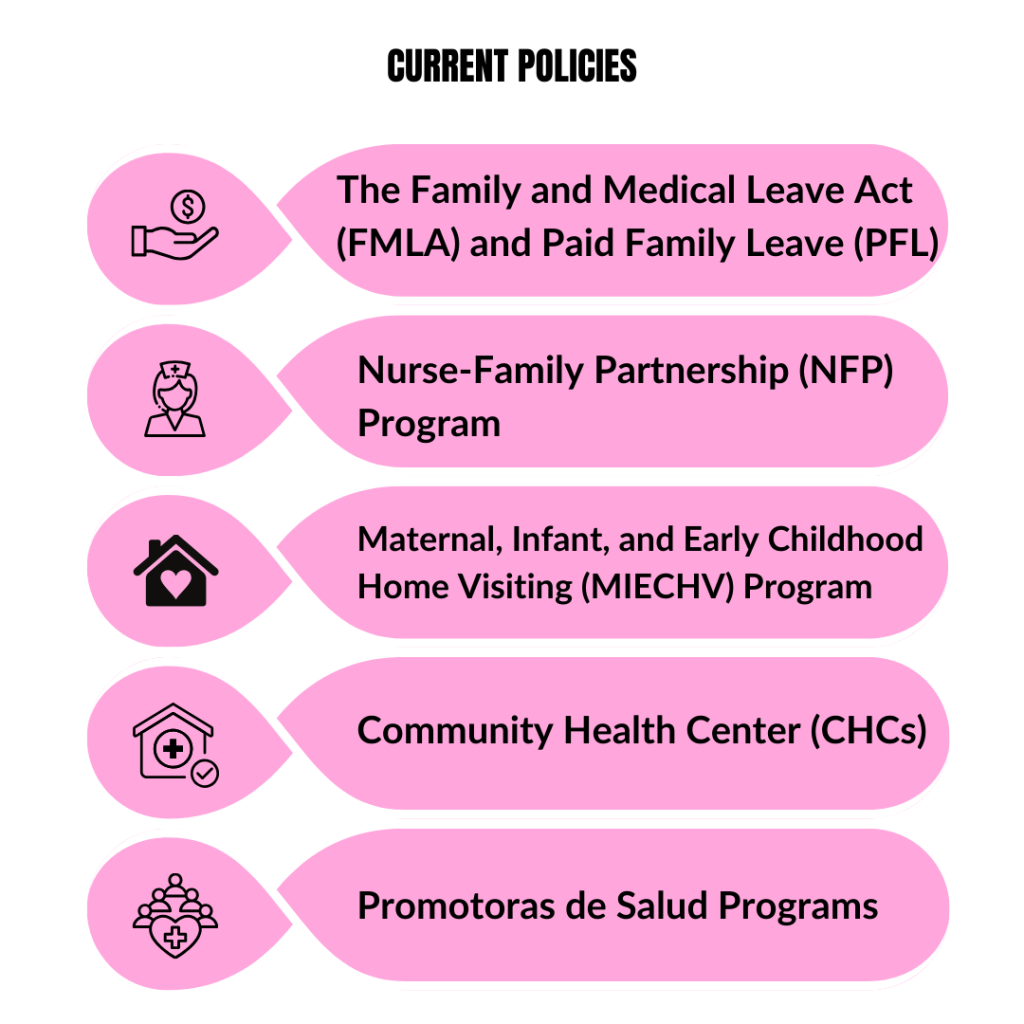
The Family and Medical Leave Act (FMLA) and Paid Family Leave (PFL)
1. What Are They?
- The Family and Medical Leave Act (FMLA), enacted in 1993, is a federal law that provides eligible employees with up to 12 weeks of unpaid, job-protected leave per year for specific family and medical reasons. abetterbalance.org
- Paid Family Leave (PFL) refers to state-level programs that offer paid leave benefits to employees for similar qualifying events, such as bonding with a new child or caring for a seriously ill family member. abetterbalance.org
2. Impact
- Job Security and Income Support: When FMLA’s job protection is combined with PFL’s income support, families can take necessary time off without fearing job loss or financial hardship, maintaining stability during family and medical events. The U.S. Department of Labor highlights that paid family and medical leave policies enable workers to receive wage replacement when they take extended time off for qualifying reasons, such as bonding with a new child or caring for a loved one with a serious health condition. dol.gov
- Improved Health Outcomes: Access to both FMLA and PFL allows caregivers to stay home with infants or care for ill family members without worrying about losing income or employment, leading to better maternal and child health, reduced stress, and enhanced emotional well-being. The American Academy of Pediatrics emphasizes that paid family and medical leave has substantial health benefits, including lower rates of preterm birth, low birth weight, and child hospital admissions; reduced neonatal, infant, and child mortality rates; higher rates of breastfeeding; and higher timely vaccination rates. marketwatch.com
- Employee Retention: The combination of PFL and FMLA can promote employee retention by allowing workers to take necessary leave and return to work, benefiting employers through reduced turnover costs and a more consistent workforce. Research indicates that paid leave benefits businesses by improving retention and productivity and boosting labor force participation. Paid leave programs in various places have shown positive impacts on employee retention. Center for Budget and Policy Priorities and National Partnership
- Gender Equality: Access to both FMLA and PFL can encourage men to take parental leave, balancing caregiving responsibilities and promoting gender parity in the workplace and family interactions. Studies have found that paid family leave programs increased the number of leaves taken by both men and women, with a significant effect on encouraging men to participate in caregiving. This shift contributes to balancing caregiving responsibilities and promoting gender equality. National Partnership
3. Why Are They Helpful?
- Comprehensive Support: The Family and Medical Leave Act (FMLA) provides eligible employees with up to 12 weeks of unpaid, job-protected leave per year for specified family and medical reasons, ensuring job protection during critical life events. dol.gov
- Paid Family Leave (PFL) programs, which vary by state, offer wage replacement benefits ranging from 50% to 100% of an employee’s average weekly wage, up to a maximum weekly benefit amount, thereby providing income replacement during such periods. ep
- Economic Stability: Financial Security for Families: PFL provides wage replacement during critical times, helping families maintain financial stability and reducing reliance on public assistance programs. dol.gov
- Reduction in Poverty Rates: Access to paid leave has been linked to decreased poverty rates among families, as it ensures continued income during periods of caregiving.
- Enhanced Economic Growth: Implementing paid family leave policies can boost economic growth by increasing labor force participation and reducing income inequality. Equitable Growth
- Public Health Benefits:
Improved Maternal and Child Health: Paid leave policies are associated with better health outcomes for mothers and children, including reduced infant mortality and higher rates of breastfeeding. National Partnership- Increased Vaccination Rates: Parents with access to paid leave are more likely to adhere to recommended vaccination schedules for their children, contributing to higher immunization rates. newamerica.org
- Enhanced Mental Health: Paid leave allows individuals to recover from illnesses or care for sick family members, reducing stress and improving overall mental health. en.wikipedia.org, pmc, stanford.edu
4. Challenges
- Limited Coverage: FMLA Exclusions: The FMLA applies to employers with 50 or more employees within a 75-mile radius, excluding many small businesses. Additionally, employees must have worked at least 1,250 hours over the past 12 months to be eligible, leaving part-time and newer employees without coverage. empowerhr.com
- Awareness and Accessibility: Many Latino families may be unaware of these benefits or face obstacles to accessing them, such as language barriers or complex enrollment processes.
- Partial Wage Replacement: PFL often provides only partial salary replacement, which can place a financial burden on low-income families that rely on their full wages to meet daily needs.
- A study by the National Center for Children in Poverty notes that many women, especially those with low incomes, may not afford to take extended time off with only partial wage replacement. nccp.org
- Research from the U.S. Department of Health and Human Services highlights that the 60 to 70 percent wage replacement offered by PFL did not meet the financial needs of most mothers, leading some to cut their leave short. aspe.hhs.gov
- State Variations: The availability and quality of PFL vary greatly between states, resulting in inequities. FMLA protects jobs but not income, and PFL programs are not universally available, leaving many families without adequate support.
- The National Center for Children in Poverty reports that, in the absence of federal legislation, 13 states and the District of Columbia have implemented or passed paid parental leave policies, with variations in eligibility, leave duration, and wage replacement rates. ncfr.org, ncfr.org
- An analysis by Family Values @ Work finds that the keys to making paid leave equitable include full access to leave, job protection for all workers, and expanded definitions of family for caregiving purposes. Child Trends, National Partnership, Child Trends
- Eligibility Restrictions: FMLA is limited to specific types of employment, such as organizations with 50 or more employees, and requires employees to meet minimum tenure criteria. This excludes many workers, particularly those in part-time, temporary, or contract jobs, where Latino and immigrant groups are frequently overrepresented. dol.govbusiness.com
Nurse-Family Partnership (NFP) Program
1. What Is It?
- The Nurse-Family Partnership (NFP) is a community-based health program that pairs registered nurses with first-time, low-income mothers, providing home visits from pregnancy through the child’s second birthday. This evidence-based program aims to improve maternal and child health, promote positive parenting, and support economic self-sufficiency. nursefamilypartnership.org
2. Impact
- Personalized Home Visits: NFP provides in-home support, which is particularly beneficial for Latina women who may face barriers accessing traditional healthcare facilities. Nurses help navigate the healthcare system and offer tailored guidance. nursefamilypartnership.org
- Improved Health Outcomes: Research shows that NFP participation leads to substantial health benefits, including a 48% reduction in child abuse and neglect, 56% fewer emergency room visits for accidents and poisonings, and a 79% decrease in preterm births among smoking mothers. nursefamilypartnership.org
- Cultural and Linguistic Support: Many NFP programs in areas with large Latino populations employ bilingual nurses or translators, ensuring Spanish-speaking mothers feel supported and understood. nursefamilypartnership.org
3. Why Is It Helpful?
- Early Intervention for Maternal and Infant Health: By beginning during pregnancy, NFP improves birth outcomes and supports early child development, reducing the likelihood of health complications later in life. mchb.hrsa.gov
- Economic Benefits for Families: Mothers who participate in NFP are more likely to achieve higher levels of education and employment, leading to long-term economic stability. For every $1 invested in NFP, states save $5.70 in future costs. sorensonimpactinstitute.com
- Reduction in Government Assistance Dependency: NFP has been shown to decrease long-term reliance on Medicaid, food assistance programs, and other public services by helping families become more self-sufficient. nursefamilypartnership.org
4. Challenges
- Limited Availability: NFP is not universally available, particularly in rural and low-income urban areas where many Latino families live. This limits the program’s reach to those who could benefit most. pmc.ncbi.nlm.nih.gov
- Restricted to First-Time Mothers: The program only serves first-time mothers, excluding many Latina mothers with multiple children who could still benefit from home visiting support. cebc4cw.org
- High Cost of Implementation: Hiring highly trained nurses and maintaining program funding can be expensive, limiting its scalability and availability, especially in areas with high demand. nursefamilypartnership.org
- NFP’s impact among Latino families that would most benefit from the program is limited since it is not offered everywhere, particularly in rural or impoverished urban areas. Nurse-Family Partnership, 2015
Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program
1. What Is It?
- The Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program is a federal initiative that supports voluntary, evidence-based home visiting services for expectant parents and families with young children up to kindergarten entry. The program aims to improve maternal and child health, prevent child abuse and neglect, encourage positive parenting, and promote child development and school readiness. Maternal and Child Health Bureau
2. Impact
- Home-Based Assistance: MIECHV provides home-based support, including health care, parenting education, and connections to community resources. This approach is particularly beneficial for Latino families who may face language or transportation challenges when accessing traditional healthcare services.
- Addressing Language and Transportation Barriers: MIECHV programs recognize that Latino families often encounter language barriers and limited transportation options, hindering access to healthcare services. By offering home-based support, MIECHV ensures that families receive essential services without the need to travel, effectively mitigating these challenges. This approach not only provides convenience but also fosters a comfortable environment for families, encouraging active participation and engagement. apha.confex.com
- Targeting Health Inequities: The program focuses on low-income and minority families, including Latinos, aiming to reduce health disparities by allocating resources to areas where they are most needed.
- Targeting High-Risk Populations: MIECHV funds are specifically allocated to high-risk populations, including low-income communities, pregnant women under 21, children with developmental delays, and families with histories of abuse, neglect, or substance abuse. This targeted funding ensures that resources are directed to those most in need, aiming to reduce health disparities and promote equitable health outcomes. PubMed Central
- Needs Assessment and Resource Allocation: States receiving MIECHV funding are required to conduct comprehensive needs assessments to identify at-risk communities. These assessments guide the allocation of resources, ensuring that home visiting programs are implemented in areas with significant maternal and child health challenges, thereby addressing systemic inequities in healthcare access and quality. Maternal and Child Health Bureau
- Culturally Relevant Support: MIECHV programs often collaborate with community health workers, such as promotoras de salud, who are familiar with Latino cultural settings and can build trust with families. Vanderbilt University CDN
3. Why Is It Helpful?
- Comprehensive Support: By providing a combination of direct services and referrals, MIECHV addresses various aspects of family well-being, including health, education, and economic self-sufficiency. Maternal and Child Health Bureau
- Early Intervention: Home visiting during pregnancy and early childhood has been shown to improve outcomes for children and families, laying a strong foundation for future development. Maternal and Child Health Bureau
4. Challenges
- Variations in Funding and Implementation: States differ in how MIECHV is funded and implemented, affecting service quality and accessibility. Latino families in states with less MIECHV support may receive lower-quality care. Congressional Research Service Reports
- Limited Reach: Due to financial limitations, only a portion of eligible families may be served by MIECHV programs, leaving many Latino families without access to services or on waiting lists.
- Service Coverage: MIECHV-funded programs reach approximately 15% of the more than 465,000 families who are likely eligible and could benefit from MIECHV services. acf.hhs.gov
- Waiting Lists: Some home visiting programs maintain waiting lists due to limited capacity, indicating that not all eligible families can be served promptly. gucchd.georgetown.edu
- Language Accessibility: While many MIECHV programs provide multilingual support, some still struggle to accommodate all families’ linguistic needs, impacting accessibility for Latino families who do not speak English. CHCS
Community Health Center (CHCs)
1. What Is It?
- Community Health Centers (CHCs) are patient-centered healthcare organizations that provide primary and preventive care to underserved populations, regardless of ability to pay. CHCs aim to reduce health disparities by offering accessible, affordable, and culturally competent care, including services tailored to Latino families. nachc.org
2. Impact
- Reducing Financial Barriers: CHCs provide affordable healthcare services, such as pediatric and prenatal care, to low-income Latino families, regardless of insurance status, removing financial barriers to essential health services. nachc.org, razafund.org
- Culturally Sensitive Care: Many CHCs employ multilingual staff and provide culturally competent care, making Spanish-speaking Latino families feel understood and fully cared for. journalofethics.ama-assn.org
- Comprehensive Services: CHCs go beyond basic medical care by offering chronic disease management, mental health services, and preventive care, all of which improve health outcomes for Latino communities especially in Latino communities. nachc.org, pmc.ncbi.nlm.nih.gov
3. Why Is It Helpful?
- Accessible Care: CHCs ensure that low-income and uninsured individuals, including many Latino families, receive essential healthcare services, regardless of financial status. nachc.org
- Community Trust: The employment of bilingual community health workers (CHWs) fosters trust and improves health outcomes for Latino communities. journalofethics.ama-assn.org
4. Challenges
- High Demand and Underfunding: CHCs experience high patient demand but often lack sufficient funding, leading to extended wait times and limited appointment availability, particularly affecting maternal and child health in Latino populations. axios.com
- Variable Funding Stability: CHCs depend on federal funding, which is subject to political shifts, impacting service availability and the ability to expand care for underserved populations. theguardian.com
- Limited Specialized Care: Some CHCs lack specialized maternal and pediatric care, requiring referrals. Many Latino families struggle with financial, transportation, or language barriers, making follow-up care difficult. tandfonline.com
Promotoras de Salud Programs
1. What Is It?
- Promotoras de Salud, or community health workers, are trusted individuals who empower their peers through education and connections to health and social resources in Spanish-speaking communities. They use their insights and knowledge of cultural norms to provide relevant health information and education to help Hispanics work through barriers they face when addressing complex health issues. mhpsalud.org
2. Impact
- Culturally Specific Health Education: Promotoras serve as cultural bridges between community-based organizations, healthcare agencies, and their respective communities, delivering health education that resonates with cultural norms and values. chhs.fresnostate.edu , chhs.fresnostate.edu
- Assistance in Navigating Healthcare Systems: Promotoras help individuals access and understand local, state, and government resources, which is crucial for low-income Latino families who might be unfamiliar with healthcare systems. mhpsalud.org
- Education on Health Behaviors: Promotoras provide health outreach and educational sessions in Spanish, including information on nutrition, prenatal and postnatal care, and other health behaviors that can improve the health of both mothers and children. mhpsalud.org
3. Why Is It Helpful?
- Trusted Community Members: Promotoras are often members of the communities they serve, allowing them to build trust and effectively disseminate health information. mhpsalud.org
- Addressing Social Determinants of Health: By providing culturally relevant health education and assistance, promotoras address social determinants of health that affect Latino communities, leading to improved health outcomes. Salud America, Pearsuite
4. Challenges
- Funding Instability: Many promotora programs depend on irregular or insufficient funding, which affects their capacity to provide communities with efficient and long-lasting services. PubMed Central
- Limited Formal Medical Training: Promotoras may not have received formal medical training, which could limit their capacity to handle urgent medical situations or complex medical demands. JSTOR
- Scope and Demand Limitations: The effectiveness of these programs in addressing the wide spectrum of requirements in Latino maternal and child health may be limited by their modest size and inability to fully fulfill demand. scholarworks.lib.csusb.edu
Policy and Programmatic Recommendations
Data-driven solutions to further minimize infectious disease spread among U.S. Latinos.
Programmatic Recommendations:
Implement Community-Based Health Education Programs
- Develop and support programs that provide culturally tailored health education to Latino communities. These initiatives should focus on preventive care, nutrition, and management of chronic conditions, utilizing community health workers or promotoras to bridge cultural and linguistic gaps. Such programs have been shown to improve health outcomes by addressing specific community needs. en.wikipedia.org
- Encourage healthy eating initiatives tailored to the community, such as community gardens, farmers’ markets, school programs, and businesses’ support of healthy foods. Participation in programs like the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) for eligible women is also recommended. NCBI
Role of Promotoras and CHCs in Education:
- Effective Collaboration: Promotoras, as trusted community health workers, play a pivotal role in delivering health education within Latino communities. Collaborating with CHCs, they can develop and disseminate culturally relevant teaching materials and conduct workshops on maternal health, effectively engaging community members. PubMed Central
- Develop Culturally Tailored Materials: Create educational resources that resonate with Latino cultural values and are available in Spanish and English to ensure accessibility.
- Train Promotoras and CHC Staff: Provide training for Promotoras and CHC personnel to effectively deliver educational content and facilitate workshops that cater to the specific needs of Latino families.
- Community Workshops: Organize interactive workshops focusing on key topics such as prenatal care, nutrition, breastfeeding, and mental health, encouraging active participation from both parents.
Expand Access to Maternal Health Services
- Increase the availability of comprehensive prenatal and postnatal care for Latino families by integrating services into community health centers and providing support through Medicaid expansion. Ensuring access to continuous care during and after pregnancy can significantly reduce maternal and infant mortality rates. en.wikipedia.org
- Support federal public policy and legislative actions aimed at improving maternal health. This includes funding for maternal health programs, developing plans to assist birth center expansion in rural and urban maternity care deserts, and ongoing funding of maternal health programs at the federal level, such as the Title V Maternal and Child Health Block Grant (MCHBG). American Hospital Association
3. Address Social Determinants of Health
- Recognize that anti-immigrant policies and practices have been linked to poorer maternal and child health outcomes among Latinos. Addressing these social determinants is crucial for improving health outcomes. PubMed Central
4. Integrate Mental Health Services into Maternal Care
- Develop strategies to incorporate mental health care into maternal health services, ensuring that expectant and new mothers have access to necessary support. This approach addresses the holistic well-being of mothers, which is crucial for positive health outcomes. SAMHSA
5. Enhance Data Collection and Analysis to Address Health Disparities
- Invest in data linkage and analysis to identify and address racial and ethnic disparities in maternal and child health outcomes. Enhanced datasets can inform targeted interventions and policies aimed at achieving health equity. ASTHO
Policy Recommendations:
Informed by Evidence: Policy Recommendations from Experts
Expand Access to Medicaid, CHIP, and ACA Benefits
Simplify the Medicaid and CHIP eligibility as well as enrollment processes to decrease documentation hurdles and frequent redetermination needs (Caraveo et al., 2021).
In places where Medicaid has not been extended, Latino families frequently encounter challenges such as difficult enrollment processes along with eligibility limitations. Simplifying Medicaid and CHIP access, particularly for prenatal along with pediatric care, would help Latino families maintain continuity of care (Whitener & Corcoran, 2021).
Standardize enrollment throughout states, extend Medicaid across all states, and fund community-based outreach initiatives to assist families in enrolling.
Increase Funding and Capacity for Community Health Centers (CHCs)
Provide more regular federal and state financing to community health centers to minimize wait times, boost appointment availability, along with expand specialist maternity and pediatric care (National Association of Community Health Centers, 2023; Community Health Worker Training, 2021).
Increase Financing and Formal Training Resources: The sustainability of promotora programs is frequently challenged by limited financial and political support within the U.S. healthcare infrastructure. Formal recognition and institutionalized payment structures are essential to sustain these initiatives. Additionally, program planners have noted the substantial time and resources required for ongoing training and quality assurance for promotoras. PubMed Central
Certification Programs in Maternal and Child Health: Establishing certification programs for promotoras in maternal and child health can enhance their ability to provide specialized care. For instance, the Texas Department of State Health Services implemented a training and certification program for promotoras, as mandated by House Bill 1864. This program aims to standardize training and integrate promotoras into the healthcare system, thereby improving the quality of care in maternal and child health services. dshs.texas.gov
Strengthen Support for Promotoras de Salud Programs
Increase Financing and Formal Training Resources: Promotoras serve as patient advocates, educators, mentors, outreach workers, and translators, acting as a bridge between diverse populations and the healthcare system. However, many promotora programs encounter sustainability challenges due to limited financial and political support within the U.S. healthcare infrastructure. Program planners have noted the substantial time and resources required for ongoing training and quality assurance for promotoras. Formal recognition and institutionalized payment structures are essential to sustain these initiatives. Rural Health Information Hub
Certification Programs in Maternal and Child Health: Establishing certification programs for promotoras in maternal and child health can enhance their ability to provide specialized care. For instance, the Texas Department of State Health Services (DSHS) offers a certification program requiring completion of a 160-hour competency-based training or verification of 1,000 hours of community health work experience. This program aims to standardize training and integrate promotoras into the healthcare system, thereby improving the quality of care in maternal and child health services. DSHS , DSHS-Regional Local Health Operations
Expand and Strengthen Home Visiting Programs:
Increase financing for the Nurse-Family Partnership (NFP) and Maternal, Infant, and Early Childhood Home Visiting (MIECHV) programs to ensure that these services are broadly accessible, particularly in high-need Latino populations.
Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program: The MIECHV Program supports voluntary, evidence-based home visiting services for expectant and new parents with children up to kindergarten entry age who live in communities at risk for poor maternal and child health outcomes. The program’s goals include:Maternal and Child Health Bureau
Nurse-Family Partnership (NFP): NFP is an evidence-based program where registered nurses provide home visits to first-time, low-income mothers, starting during pregnancy and continuing through the child’s second birthday. The program aims to improve prenatal health, child health and development, and the economic self-sufficiency of families. Research has shown that NFP participants experience:NFP, NFP
Addressing Health Disparities in Latino Communities:
Latino communities often face unique challenges, including language barriers, socioeconomic disparities, and limited access to culturally competent healthcare. Evidence-based home visiting programs like NFP and MIECHV can help reduce these disparities by providing mothers with screenings, case management, family support, and referrals that address a family’s physical, mental, and health-related social needs. CHCS, CHCS
Target government money to expand program reach, especially in Latino-populated and rural regions, and hire more multilingual and culturally competent house visits.
Despite their established efficacy in improving mother and infant health, Latino families living in rural or disadvantaged urban areas may be unable to access these programs. The Commonwealth Fund, 2024b
Target Government Funding to Expand Program Reach:
The Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Program, established under the Affordable Care Act, represents a significant federal investment in home visiting services. However, current funding levels allow these programs to serve only a fraction of eligible families. For instance, in Fiscal Year 2022, MIECHV served approximately 15% of the more than 465,000 eligible families, indicating a substantial gap between need and available resources. To address this, policy recommendations include increasing federal funding to expand the reach of evidence-based home visiting programs, especially in high-need areas. PubMed Centralhrsa.gov
Hire More Multilingual and Culturally Competent Home Visitors
Implementing culturally responsive, community-driven, and anti-racist approaches in home visiting programs can enhance their effectiveness in serving diverse populations. Strategies to achieve this include recruiting and retaining home visitors who reflect the cultural and linguistic backgrounds of the communities they serve. This alignment can improve communication, trust, and program outcomes. Resources such as the reflection and planning tool provided by MIECHV can assist programs in infusing cultural and linguistic competence into their workforce development efforts. CHCS, CHCS
Implement Paid Family Leave and Expand FMLA Access
Expand FMLA to Include All Employers and Workers
Inclusion of Small Firms and Part-Time Workers: The Job Protection Act proposes extending FMLA protections to employees of small businesses with fewer than 50 employees and eliminating the 1,250-hour requirement, thereby covering part-time and multi-job workers. underwood.house.gov
Sliding-Scale Benefits: Recent state programs have adopted sliding-scale approaches to provide higher wage replacement rates for lower-wage workers, making leave more accessible and affordable. newamerica.org
Universal Paid Leave Support: The Center on Budget and Policy Priorities advocates for a permanent, national paid family and medical leave program to ensure comprehensive coverage across all states. Center for Budget and Policy Priorities, National Partnership
Employer Tax Credits: The Paid Family and Medical Leave Business Tax Credit assists employers in offering paid leave by offsetting associated costs, thereby supporting small businesses in providing these benefits. Bipartisan Policy. National Policy
Expand Access to WIC Services and Extend Coverage
Extend the WIC program’s eligibility period to provide nutritional needs throughout the early years, and expand outreach efforts in remote regions.
WIC increases child and maternal nutrition, but it only covers certain life stages, and certain families that qualify living in rural or impoverished regions have restricted access. Caraveo et al., 2021
Extend WIC coverage to include additional developmental years, and provide portable or community-based WIC programs to reach isolated Latino populations.
Increase Accessibility and Cultural Competency in ACA Marketplace Plans
Improve navigation assistance for ACA Marketplace plans, including language support and digital literacy materials, to aid Latino families in enrolling and using insurance. InsureKidsNow, 2024
Language hurdles and computer literacy issues might make it difficult for Latino families to understand their ACA options and obtain preventative care.
Collaborate with community groups to offer multilingual ACA navigators along with online tools that assist families in understanding their healthcare options as well as completing the enrollment process.
Call to Action: Get Involved
Strengthening Maternal and Child Health in Latino Communities
Latino maternal and child health disparities demand urgent action. The current healthcare system fails to fully meet the needs of Latino families, putting the future health and well-being of mothers and children at risk. We must advocate for systemic changes that expand healthcare access, enhance cultural competency, and prioritize the health of Latina women and their families.
For Decision-Makers & Policymakers:
- Expand Access to Healthcare: Support policies that increase Medicaid, CHIP, and MIECHV funding to ensure Latino families receive prenatal, postnatal, and pediatric care.
- Strengthen Workforce Diversity: Invest in the recruitment and training of bilingual, culturally competent healthcare providers, including Promotoras de Salud and community health workers.
- Improve Paid Leave Protections: Push for expanded FMLA coverage and national Paid Family Leave policies to help working Latino parents care for newborns without financial hardship.
- Fund Culturally Relevant Health Education: Support community-based initiatives that provide Spanish-language health resources and workshops on maternal wellness, breastfeeding, and mental health.
For Families & Community Leaders:
- Stay Informed & Advocate: Learn about your healthcare rights, access available resources, and share information with your community. Contact local representatives to demand action on maternal and child health policies.
- Engage in Community Programs: Participate in maternal health initiatives, such as Promotoras-led workshops or CHC services, to access trusted, culturally relevant care.
- Support Maternal Health Organizations: Volunteer with or donate to groups working to improve healthcare access and outcomes for Latino mothers and children.
The health of Latina women and children is the foundation of our communities. Now is the time to act—whether by advocating for legislative change, supporting local health organizations, or helping families navigate the healthcare system. Together, we can ensure a healthier future for Latino families.
Partners and Resources for Families
Please see below for key resources to use for your family.
🌍 Key Resources for Families
There are numerous organizations and programs that provide culturally competent support, from financial assistance and family planning services to maternal health education and early childhood development programs. Whether you need guidance on healthcare access, breastfeeding, mental health support, or parenting, these resources are designed to help Latino families thrive.
Explore national and local programs that can connect you to the care and support your family needs.
Have questions on how to apply for these resources– see below:
Head Start Program
The Head Start Program provides comprehensive early childhood education, nutrition, and family support services for low-income families. Designed to prepare young children for school, Head Start also offers resources for parents, including health screenings, social services, and parental engagement programs. Families can apply for Head Start in their local area to ensure their children receive quality early education and support.
🔹 Apply here: Find a Head Start Center Near You

WIC Program (Women, Infants, and Children)
The WIC Program provides nutritional support, breastfeeding assistance, and health screenings for pregnant women, new mothers, and children under 5. Families enrolled in WIC receive monthly food benefits, nutrition education, and referrals to healthcare services to promote healthy growth and development. This federally funded program is available in all states and territories.
🔹 Apply here: Find Your Local WIC Office
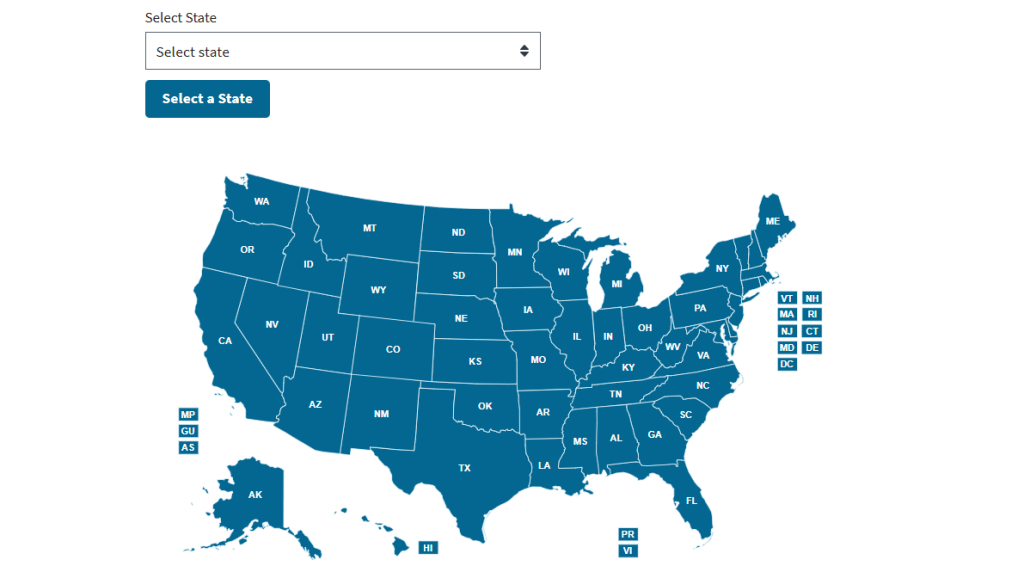
Medicaid and CHIP (Children’s Health Insurance Program)
Medicaid and CHIP provide low-cost or free health coverage for eligible children, pregnant women, and low-income families. These programs cover doctor visits, immunizations, prescriptions, hospital care, and more. Each state runs its Medicaid and CHIP programs with its own eligibility requirements, so it’s important to check your state’s specific guidelines.
🔹 Apply here: Find Medicaid & CHIP Programs in Your State
Need Health Insurance? Enroll Through the Marketplace
If you don’t qualify for Medicaid or CHIP, you can find affordable health coverage through the Health Insurance Marketplace. Plans cover essential health benefits like preventive care, maternity care, and prescriptions, and financial assistance is available for those who qualify. Open enrollment happens yearly, but special enrollment periods exist for major life events like pregnancy or loss of other coverage.
🔹 Apply here: Get Health Coverage Through the Marketplace
Find additional resources below:
Click Here for Additional Resources
Health Resources and Services Administration (HRSA):
- Provides healthcare services to economically or medically vulnerable populations, including programs for pregnant individuals, mothers, and families.content.govdelivery.com
- Website: HRSA Maternal and Child Health
National Latina Institute for Reproductive Justice:
- Advocates for reproductive health and justice for Latinas through education, policy advocacy, and community mobilization.en.wikipedia.org
- Website: National Latina Institute
AVANCE:
- Offers parenting and early childhood education programs to low-income, predominantly Hispanic families, focusing on children up to three years old.en.wikipedia.org
- Website: AVANCE
Every Body Texas:
- Connects individuals with low-cost family planning and preventive health services, including birth control and STI testing.everybodytexas.org+1cameroncountytx.gov+1
- Find a clinic: Every Body Texas Clinic Finder
2-1-1 Website:
- For assistance in identifying local resources, including financial help, the 2-1-1 helpline is a valuable tool. This free, confidential service is available 24/7 across the United States and connects individuals to essential community services, such as housing assistance, food programs, and health care resources.
- Reach the helpline here: Dial 211 or Visit the 2-1-1 website.
Planned Parenthood:
- Offers prenatal care referrals, birth control, STI testing, and fertility services to ensure family planning options for all.
- To find a health center near you, visit their Health Center Locator.
🌍 Additional Resources and Data for Partners
Partners play a vital role in maternal and child health by providing emotional, financial, and physical support to expectant and new mothers. However, they may not always have access to the information and resources they need to be active participants in their family’s well-being. These partner-focused resources offer guidance on parenting, mental health, and healthy relationships while promoting engagement in maternal and child health. Whether you’re a father, co-parent, or caregiver, these resources can help you better support your loved ones during pregnancy, childbirth, and beyond.
Click here to view all Partner-related Resources:
March of Dimes
Website: https://www.marchofdimes.org/
Description: Focuses on maternal and baby health by addressing concerns such as preterm, birth deformities, and infant mortality. The March of Dimes promotes mother and child health via education, advocacy, as well as community activities, with a focus on at-risk communities such as Latino families.
National Hispanic Medical Association (NHMA)
Website: https://www.nhmamd.org/
Description: Works to enhance healthcare access in Hispanic populations. The NHMA collaborates with healthcare providers to improve health disparities, especially mother and child health, including offers tools as well as advocacy for care that is culturally competent.
Migrant Clinicians Network (MCN)
Website: https://www.migrantclinician.org/
Description: Supports healthcare access to migratory and underserved groups, primarily Latino families, with a particular emphasis on child and maternal health. MCN offers healthcare services, mobile clinics, as well as materials for prenatal care and healthy pregnancy.
Nurse-Family Partnership (NFP)
Website: Nurse Family Partnership
Description: A program that pairs nurses with first-time, low-income moms to promote prenatal health, child development, as well as maternal self-sufficiency. NFP customizes programs to match the cultural needs of Latino women, allowing them to access healthcare and other resources.
Planned Parenthood
Website: Planned Parenthood
Description: Community health worker initiatives aimed to provide culturally appropriate health services and education to Latino populations. Promotoras play an important role in the well-being of mothers and babies by assisting families with accessing healthcare, comprehending nutrition, and handling care prior to and after delivery.
To find a health center near you, visit their Health Center Locator.
The Healthy Start
Website: https://mchb.hrsa.gov/programs-impact/healthy-start
Description: Aims to improve maternal and newborn health outcomes in high-risk communities. The program aims to reduce infant mortality, provide healthcare during pregnancy and afterwards, and provide culturally appropriate services to marginalized communities, including Latinos.
Additional HRSA Programs: https://mchb.hrsa.gov/programs-impact/programs
National Association of Community Health Centers (NACHC)
Website: What Is a Health Center?
Community Health Centers provide affordable, high-quality healthcare to millions of people, regardless of income or insurance status. These centers offer primary care, prenatal and pediatric services, mental health support, and preventive screenings in underserved and rural communities. Many centers have multilingual staff and culturally competent care, making them essential for Latino families seeking accessible healthcare.
National Latino Network for Healthy Families and Communities
Website: National Latino Network
This organization offers resources and training focused on promoting healthy relationships and preventing domestic violence within Latino communities. They provide culturally specific materials that can help partners support maternal and child health.
MHP Salud
Website: MHP Salud Health Education Resources
MHP Salud develops culturally competent health education materials specifically for underserved Latino communities. Their resources cover various topics, including maternal and child health, and can be valuable for partners seeking to support their families.mhpsalud.org
Hispanic Health Council
Website: Hispanic Health Council
This organization offers programs and services designed to improve healthy lifestyles, including nutrition and physical activities, across the life course in socioeconomically vulnerable communities. Their resources can help partners understand and support maternal and child health needs.hispanichealthcouncil.org
Center for Latino Adolescent and Family Health (CLAFH)
Website: CLAFH
CLAFH aims to reduce health disparities and improve the overall well-being of Latino adolescents and their families. They offer resources and research that can guide partners in supporting maternal and child health.
AVANCE
Website: AVANCE
AVANCE provides parenting and early childhood education programs to low-income, predominantly Hispanic families. Their resources can help partners engage in their children’s development and support maternal health.
References
Click here to review all relevant references.
Betancourt, J. R. (2024, December 17). Hispanic/Latino adults lack adequate, affordable health insurance coverage. The Commonwealth Fund. https://www.commonwealthfund.org/blog/2024/hispaniclatino-adults-lack-adequate-affordable-health-insurance-coverage?utm_source=
Caraveo, C. A., Basurto, L. E., Gonzalez, D., & Pan, C. W. (2021). Barriers to Medicaid and CHIP coverage for eligible but uninsured latinx children. Urban Institute. https://www.urban.org/research/publication/barriers-medicaid-and-chip-coverage-eligible-uninsured-latinx-children?utm_source=
Centers for Disease Control and Prevention. (2022, November 7). Maternal mortality rates in the United States, 2020 (D. L. Hoyert, Ed.). National Center for Health Statistics. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2020/maternal-mortality-rates-2020.htm
CLASP. (2016, February 17). New analysis of access to child care subsidies, head start finds disparate access by race, ethnicity, and state. CLASP. https://www.clasp.org/press-room/press-releases/new-analysis-access-child-care-subsidies-head-start-finds-disparate-access-race-ethnicity-and-state/?utm_source=
Community Health Worker Training. (2021, August 27). How community health workers can support your maternal and child health program – Community health worker training. CHW Training. https://chwtraining.org/maternal-child-health-program-chws/?utm_source=
Coombs, B. (2023, October 13). The U.S. has high maternal mortality rates — and it has gotten worse for Latinas. CNBC. https://www.cnbc.com/2023/10/13/pregnant-latinas-face-greater-maternal-health-concerns.html
Despres, C. (2023, November 1). Food insecurity on the rise in America, especially among Latinos. Salud America. https://salud-america.org/food-insecurity-on-the-rise-in-america-especially-among-latinos/
Drake, P., Tolbert, Jennifer, Rudowitz, R., Damico, A., & Kaiser Family Foundation. (2024, February 26). How Many Uninsured Are in the Coverage Gap and How Many Could be Eligible if All States Adopted the Medicaid Expansion? KFF. https://www.kff.org/medicaid/issue-brief/how-many-uninsured-are-in-the-coverage-gap-and-how-many-could-be-eligible-if-all-states-adopted-the-medicaid-expansion/
Fryer, K., Lewis, G., Munoz, C., & Stuebe, A. M. (2021). Identifying barriers and facilitators to prenatal care for Spanish-speaking women. North Carolina Medical Journal, 82(1), 7–13. https://doi.org/10.18043/ncm.82.1.7
Harris, R. A., & Santos, H. P., Jr. (2020). Maternal depression in Latinas and child socioemotional development: A systematic review. PloS One, 15(3), e0230256. https://doi.org/10.1371/journal.pone.0230256
Hoyert, D. L. (2024, May 1). Maternal mortality rates in the united states, 2022. National Center for Health Statistic. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2022/maternal-mortality-rates-2022.htm
InsureKidsNow. (2024). Inclusive outreach. InsureKidsNow.Gov. https://www.insurekidsnow.gov/initiatives/inclusive-outreach?utm_source=
Lin, K. (2022, September 19). The evidence is in: WIC improves maternal and child health. American Academy of Family Physicians. https://www.aafp.org/pubs/afp/afp-community-blog/entry/the-evidence-is-in-wic-improves-maternal-and-child-health.html?utm_source=
Lukens, G., & Harker, L. (2024, July 9). Closing medicaid coverage gap would help diverse groups and reduce inequities. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-help-diverse-groups-and-reduce-inequities?utm_source=
March of Dimes Perinatal Data Center. (2024). Fertility rates by race/ethnicity: United States, 2021-2023 Average. March of Dimes | PeriStats. https://www.marchofdimes.org/peristats/data?reg=99&top=2&stop=4&lev=1&slev=1&obj=1
National Association of Community Health Centers. (2023, June 22). Maternal health. NACHC. https://www.nachc.org/topic/maternal-health/?utm_source=
National Head Start Association. (2022). Head Start united: Removing barriers to access for children and families. Research Connections. https://researchconnections.org/childcare/resources/136631?utm_source=
Nurse-Family Partnership. (2015, October). NURSE-FAMILY PARTNERSHIP’S National Results of the Maternal, Infant, and Early Childhood Home Visiting Program. Nurse-Family Partnership.Org. https://www.nursefamilypartnership.org/wp-content/uploads/2018/04/2015NFP_MIECHVReport_forprint-1.pdf
Obstetrics & Gynecology. (2020). Racial and ethnic disparities in perinatal insurance… : Obstetrics & gynecology. LWW. https://journals.lww.com/greenjournal/fulltext/2020/04000/racial_and_ethnic_disparities_in_perinatal.20.aspx
Office of Minority Health. (2024, October 29). Infant mortality and Hispanic Americans. U.S. Department of Health & Human Services. https://minorityhealth.hhs.gov/infant-mortality-and-hispanic-americans
Policy Center For Maternal Mental Health. (2023, October 25). Fact sheet: Maternal mental health. Policy Center for Maternal Mental Health. https://policycentermmh.org/maternal-mental-health-fact-sheet/?utm_source=
Ramirez, L., Guzman, L., & Alvira-Hammond, M. (2024, October 9). Latino children represent at least 1 in 4 kids nationwide, and more than 40 percent in 5 states and Puerto Rico. Hispanic Research Center. https://www.hispanicresearchcenter.org/research-resources/latino-children-represent-1-in-4-kids-nationwide/
Sonchak, L. (2016). The impact of WIC on birth outcomes: New evidence from South Carolina. Maternal and Child Health Journal, 20(7), 1518–1525. https://doi.org/10.1007/s10995-016-1951-y
The Commonwealth Fund. (2024a, June 4). Insights into the U.S. maternal mortality crisis: An international comparison. Commonwealth Fund. https://www.commonwealthfund.org/publications/issue-briefs/2024/jun/insights-us-maternal-mortality-crisis-international-comparison
The Commonwealth Fund. (2024b, December 3). Improving maternal and infant health through multisector, community-driven partnerships. Commonwealth Fund. https://www.commonwealthfund.org/publications/fund-reports/2024/dec/improving-maternal-infant-health-community-partnerships?utm_source=
U.S. Department of Agriculture. (2024, December 13). About WIC. Food and Nutrition Service. https://www.fns.usda.gov/wic/partner/about
U.S. Department of Health and Human Services. (2019, April 29). Latino children in head start: Family characteristics, parent involvement, and satisfaction with the head start program. The Administration for Children and Families. https://www.acf.hhs.gov/opre/training-technical-assistance/latino-children-head-start-family-characteristics-parent?utm_source=
U.S. Department of Health and Human Services. (2022). Infant mortality and Hispanic Americans. Office of Minority Health. https://minorityhealth.hhs.gov/infant-mortality-and-hispanic-americans
Villagra, M. V. G., Bhuva, B., Coman, E., Smith, M. D. O., & Fifield, J. (2019, March 7). Health insurance literacy: Disparities by race, ethnicity, and language preference. AJMC. https://www.ajmc.com/view/health-insurance-literacy-disparities-by-race-ethnicity-and-language-preference?utm_source=
Whitener, K., & Corcoran, A. (2021, June 8). Getting back on track: A detailed look at health coverage trends for Latino children. Center For Children and Families. https://ccf.georgetown.edu/2021/06/08/health-coverage-trends-for-latino-children/?utm_source=
American Hospital Association. (2024, September 28). Federal public policy and legislative solutions improving maternal health. https://www.aha.org/advocacy/2024-09-28-federal-public-policy-and-legislative-solutions-improving-maternal-health
American Academy of Family Physicians. (2022, September 19). The evidence is in: WIC improves maternal and child health. https://www.aafp.org/pubs/afp/afp-community-blog/entry/the-evidence-is-in-wic-improves-maternal-and-child-health.html
Centers for Disease Control and Prevention. (2022). Maternal mortality rates in the United States, 2020. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2020/maternal-mortality-rates-2020.htm
Center for Budget and Policy Priorities. (2024). A national paid leave program would help workers & families. https://www.cbpp.org/research/economy/a-national-paid-leave-program-would-help-workers-families
Congressional Research Service Reports. (2023). State variation in maternal health outcomes and policy. https://crsreports.congress.gov
Commonwealth Fund. (2024). Improving maternal and infant health through multisector, community-driven partnerships. https://www.commonwealthfund.org/publications/fund-reports/2024/dec/improving-maternal-infant-health-community-partnerships
Duke University Center for Latino Adolescent and Family Health. (2024). Programs for Latino families. https://socialwork.duke.edu/research/centers-and-initiatives/center-latino-adolescent-and-family-health
Georgetown University Center for Children and Families. (2021, June 8). Health coverage trends for Latino children. https://ccf.georgetown.edu/2021/06/08/health-coverage-trends-for-latino-children
Health Resources and Services Administration (HRSA). (2024). Home visiting program: Maternal, Infant, and Early Childhood Home Visiting (MIECHV). https://mchb.hrsa.gov/sites/default/files/mchb/programs-impact/home-visiting/miechv-2023-rtc-letters.pdf
Hispanic Health Council. (2024). Community health initiatives. https://hispanichealthcouncil.org
March of Dimes. (2024). Fertility rates by race/ethnicity: United States, 2021-2023 Average. https://www.marchofdimes.org/peristats/data
Migrant Clinicians Network. (2024). Healthcare access for migratory and underserved populations. https://www.migrantclinician.org
National Hispanic Medical Association. (2024). Programs for improving Hispanic healthcare access. https://www.nhmamd.org
National Latina Institute for Reproductive Justice. (2024). Reproductive health and justice for Latinas. https://www.latinainstitute.org
National Partnership for Women & Families. (2024). Paid leave is essential for economic stability. https://nationalpartnership.org/report/paid-leave-good-for-business
Nurse-Family Partnership. (2022). Research trials and outcomes: Improving maternal and child health. https://www.nursefamilypartnership.org/wp-content/uploads/2022/03/NFP-Research-Trials-and-Outcomes.pdf
Office of Minority Health. (2024). Infant mortality and Hispanic Americans. U.S. Department of Health & Human Services. https://minorityhealth.hhs.gov/infant-mortality-and-hispanic-americans
Policy Center for Maternal Mental Health. (2023). Latina and Hispanic maternal mental health issue brief. https://policycentermmh.org/latina-and-hispanic-maternal-mental-health-issue-brief/
Planned Parenthood. (2024). Promotoras de Salud: Community health education programs. https://www.plannedparenthood.org/es/temas-de-salud/para-educadores/promotorxs-de-salud
Rural Health Information Hub. (2024). The role of promotoras in improving Latino health outcomes. https://www.ruralhealthinfo.org/toolkits/community-health-workers
SAMHSA. (2024). Maternal mental health strategy. https://www.samhsa.gov/sites/default/files/mmh-strategy.pdf
Salud America. (2023). Latino childhood development & healthy lifestyles. https://salud-america.org/latino-childhood-development-research-healthy-lifestyles/
Texas Department of State Health Services. (2024). Promotoras certification programs. https://www.dshs.texas.gov/community-health-worker-or-promotora-training-certification-program
U.S. Department of Agriculture. (2024). WIC program eligibility and benefits. https://www.fns.usda.gov/wic/partner/about
U.S. Department of Health and Human Services. (2022). Racial and ethnic disparities in perinatal insurance. https://www.hhs.gov
Underwood, L. (2024). Job Protection Act: Expanding FMLA protections for workers. https://underwood.house.gov/media/press-releases/job-protection-act-expansion-fmla
World Health Organization. (2024). Social determinants of health and maternal outcomes. https://www.who.int/health-topics/social-determinants-of-health
