SEXUAL HEALTH
A Call for Comprehensive and Culturally Sensitive Sexual Health Education
What is Sexual Health?
Sexual health is a vital part of our overall well-being—impacting not just physical health, but also mental, emotional, and social health. For Latino communities, sexual health includes access to the information, care, and support needed to make informed decisions and live healthy, empowered lives.
Yet deep disparities remain. Latino communities continue to face:
- High rates of sexually transmitted infections (STIs)
- Teenage and unplanned pregnancies
- Limited access to culturally relevant sexual education
- Barriers to early care for unintended or early pregnancies
These gaps are not just health issues—they are deeply tied to education, stigma, economic opportunity, and systemic inequities in healthcare access. Addressing sexual health in Latino communities means ensuring youth, families, and individuals have access to education, prevention, and care—grounded in respect, language access, and cultural understanding.
Sexual health is not just about preventing illness. It’s about knowledge, choice, dignity, and access.
High-Level Challenges:
1. Health Disparities
Latinos often face significant barriers to sexual health care, including language gaps, fear of deportation, and lack of affordable coverage. Many lack access to culturally and linguistically appropriate services, making it harder to navigate sensitive topics like STIs and contraception. Without insurance or preventive care, risks for unplanned pregnancies and untreated STIs increase. KFF: Health Coverage and Care of Immigrants, Office of Minority Health: Hispanic/Latino Health, CDC: STDs in Racial and Ethnic Minorities
2. Economic Inequities
Many Latinos work in low-wage jobs that do not offer health benefits, limiting their ability to afford healthcare. For families living paycheck to paycheck, healthcare costs often take a back seat to essentials like housing and food. Without consistent access to affordable services, individuals are more vulnerable to untreated STIs, unintended pregnancies, and other preventable outcomes. U.S. Bureau of Labor Statistics: Hispanic Employment Statistics, National Institutes of Health: Latino Health Disparities
3. Cultural Stigma & Representation
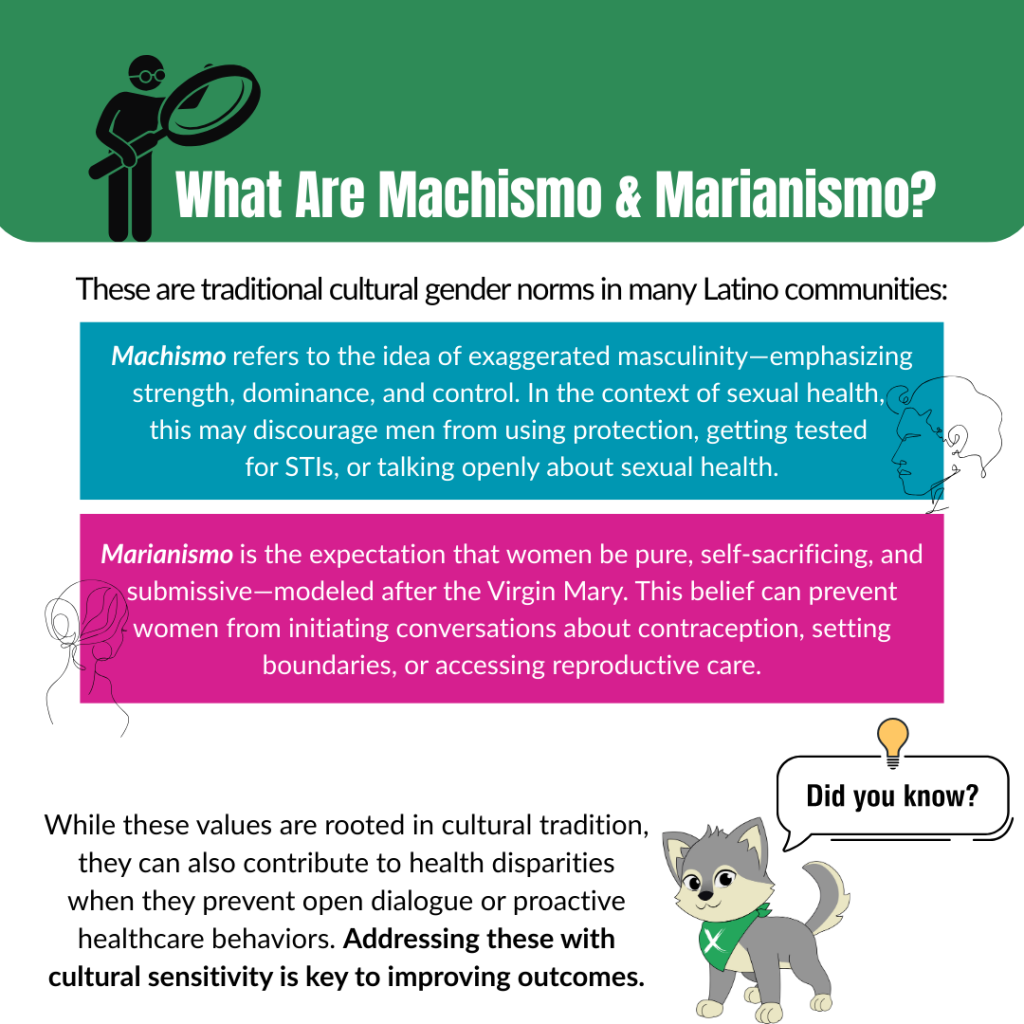
Cultural beliefs and gender roles shape how sexual health is discussed in Latino communities. Stigma around STIs, contraception, and sexuality can prevent open conversations and delay care. Norms like machismo and marianismo may discourage condom use or STI testing, especially for women and youth. Creating culturally respectful and identity-affirming interventions is key to increasing health engagement. Planned Parenthood: Talking About Sexual Health in Latino Communities, Journal of Racial and Ethnic Health Disparities: Cultural Beliefs and Sexual Health
4. Limited Access to Sexual Health Education
Many Latino youth receive limited or abstinence-only sex education, leaving gaps in knowledge about safe sexual practices. Spanish-speaking families often lack access to resources in their language, and higher dropout rates—driven by economic or family pressures—further reduce exposure to essential health education. CDC: Youth Risk Behavior Survey (YRBS), Guttmacher Institute: Sex Education and the Latino Community, Pew Research: Latino Education and Dropout Trends
Why This Issue Is Important to Latinos
Latino communities face unique and overlapping challenges when it comes to sexual health, including stigma, limited access to care, lack of comprehensive education, and broader health inequities. These challenges contribute to disproportionate rates of STIs, HIV, and reproductive health complications.
Subtopic 1- HPV & Cervical Cancer
Over 40% of Hispanic/Latinx individuals have a current genital HPV infection, and Latinas are 70% more likely to die from cervical cancer than non-Hispanic white women (Reiter et al., 2020; Shokar et al., 2020). Persistent HPV infection—often preventable through vaccination and regular screenings—remains a major health risk. But many Latinas face barriers to accessing gynecological care due to insurance status, fear, or language gaps.
Subtopic 2- HIV & STIs
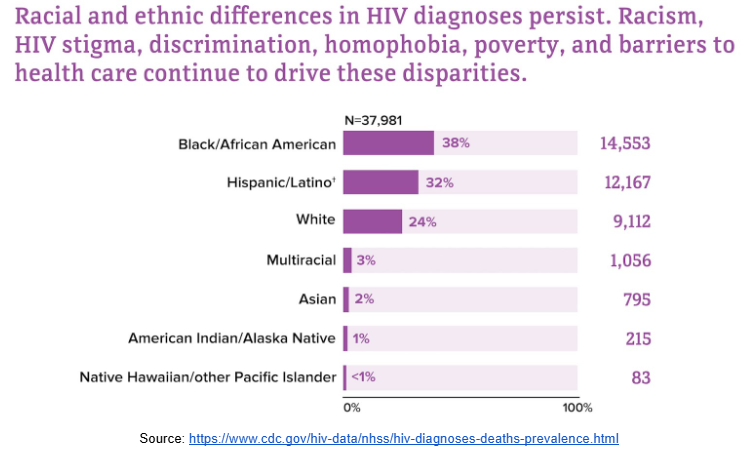
Hispanic/Latino males represented 36% of all new HIV infections among men in 2022, with rates five times higher than white males (HIV.gov, 2024a). HIV and other STIs continue to impact Latino communities at alarming rates, especially among men who have sex with men and underserved youth. These disparities reflect ongoing barriers in access to testing, prevention education, and culturally appropriate care.
Subtopic 3- Access & Stigma
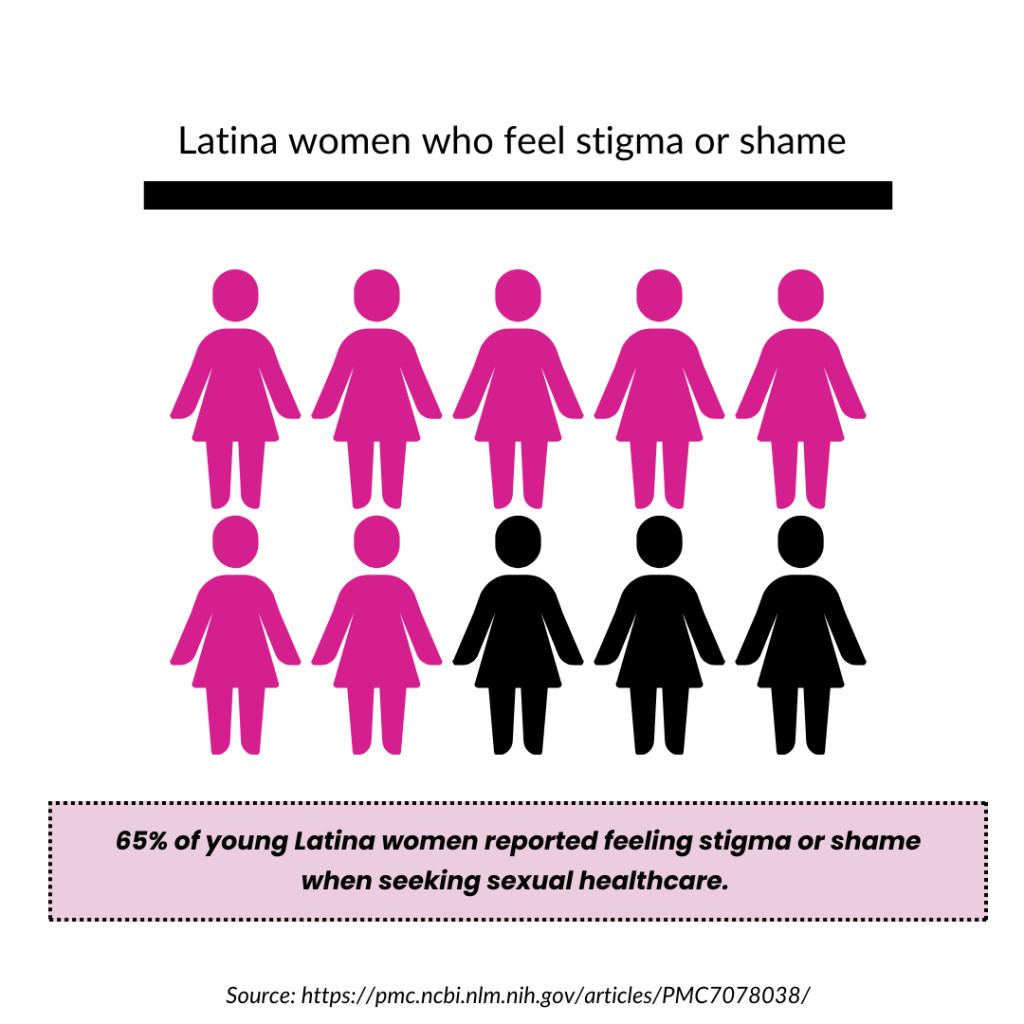
65% of young Latina women reported feeling shame or stigma when seeking sexual healthcare, and 25% of Latino patients with limited English proficiency reported difficulty scheduling appointments (Morales-Alemán et al., 2019; Escobedo et al., 2023). Cultural stigma, gender roles, and language barriers create hesitancy around accessing care or discussing sexual health. These issues are intensified by a lack of bilingual providers and inclusive care settings, leaving many without the support they need.

Data: Key Statistics
The data presented below highlights severe health disparities and obstacles to sexual healthcare within the Latino community, with a particular focus on sexual minority Latinos and young Latina women. These figures underscore the elevated risk of HIV and sexually transmitted infections (STIs), as well as barriers to care and poor reproductive health outcomes. By examining these statistics, we can better understand the critical need for expanded healthcare access, comprehensive education, and culturally sensitive solutions to address the unique challenges faced by the Latino population within the United States.
The following data highlights the disparities and barriers impacting sexual health outcomes within Latino communities—especially among women, youth, and sexual minority populations.
HPV & Cervical Cancer
- Over 40% of Hispanic/Latinx women and men have a current genital HPV infection. (Reiter et al., 2020)
- Latinas are 70% more likely to die from cervical cancer than non-Hispanic white women. Persistent HPV infection is the primary cause. (Shokar et al., 2020)
HIV & AIDS
- Latino males accounted for 36% of all new HIV infections among U.S. males in 2022 — 5x higher than white males. (HIV.gov, 2024a)
- Hispanic females were 19x more likely to have AIDS in 2022 and 3x more likely to die from HIV than white females. (Office of Minority Health, 2024)
- Hispanic males were nearly 2x more likely to die of HIV compared to white males. (Office of Minority Health, 2024)
- In 2020, 27% of HIV diagnoses in the U.S. were among Hispanic/Latino adults and adolescents. (Padilla et al., 2023)
Sexual Minority Latinos
- Gay, lesbian, and bisexual Latinos are 2.5x more likely to contract HIV compared to heterosexual peers.(Martinez et al., 2017)
- GLB Latinos also report higher rates of substance use and smoking, increasing HIV/STI risk.
Other STIs
- Hispanics had a congenital syphilis rate 3.3x higher than whites in 2018. (CDC, 2024)
- In 2018, reported gonorrhea cases among Hispanics were 1.6x higher than among whites. (CDC, 2024)
Access & Systemic Barriers
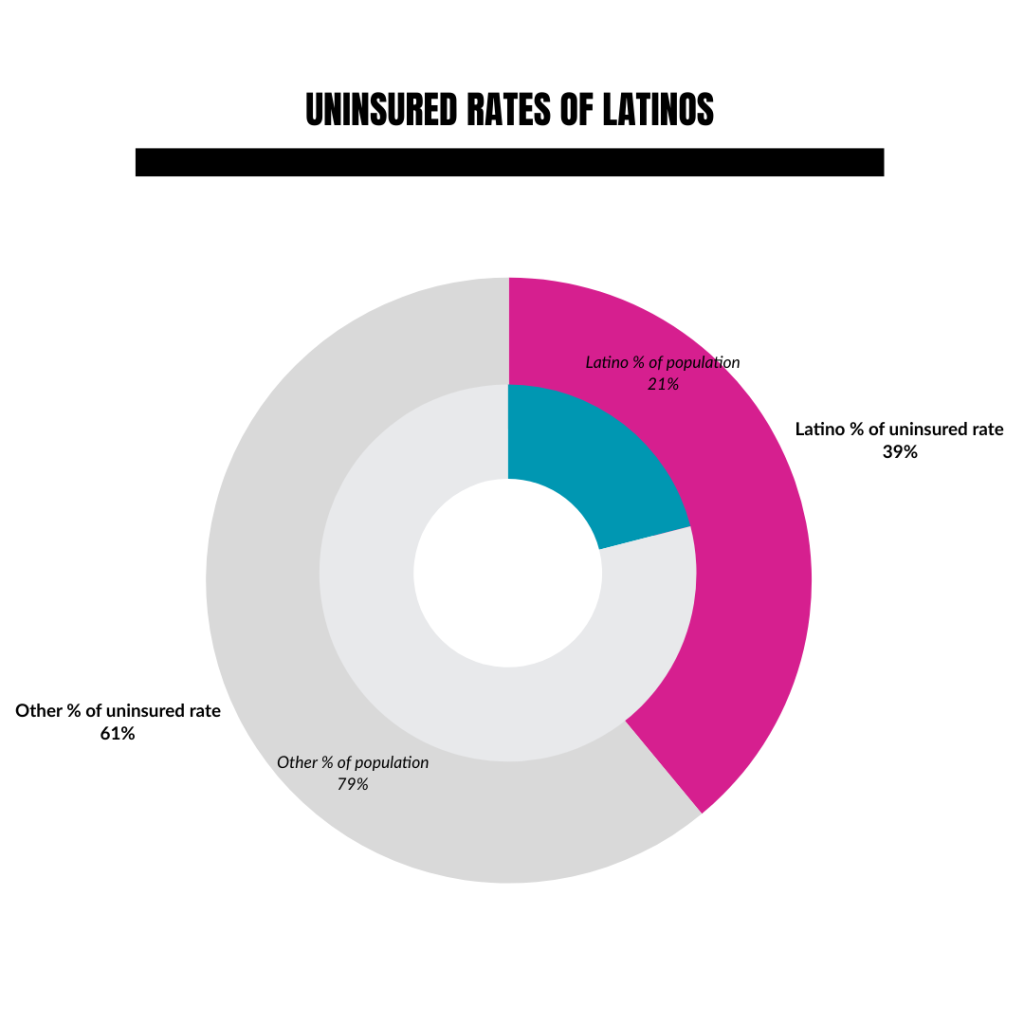
- In 2022, Latinos made up 21% of the U.S. nonelderly population but 39% of the uninsured — over twice the uninsured rate of white non-Latinos. (ASPE, 2024)
- 64% of Latino adults report worry about medical bills.(ASPE, 2024)
Language & Discrimination
- 25% of Spanish-speaking patients said they had trouble scheduling appointments, and 29% felt their condition was unresolved after a visit — compared to only 10% of English-speaking patients. (Morales-Alemán et al., 2019; Escobedo et al., 2023)
- 65% of young Latina women reported feeling stigma or shame when seeking sexual healthcare. (Morales-Alemán et al., 2019)
YOUTH IMPACT
- More than 1 in 4 Latina teens become pregnant at least once before age 20 — one of the highest rates among all racial/ethnic groups. (Power to Decide, 2023)
- Among youth ages 13–24, Hispanic/Latino individuals had the second-highest number and rate of HIV diagnoses in 2022 (2,124 cases; 16.3 per 100,000). The prevalence rate was 4.5x higher than that of white youth. (KFF, 2024)
- Among youth ages 13–24, Hispanic/Latino individuals had the second-highest number and rate of HIV diagnoses in 2022 (2,124 cases; 16.3 per 100,000). The prevalence rate was 4.5x higher than that of white youth. (KFF, 2024)
Youth Impact
- Latinas aged 15–19 had the highest teen birth rate of any racial/ethnic group in 2021 at 22.8 births per 1,000, compared to 11.4 among white teens. (CDC, 2022)
- Latino teens are more likely to report not using any contraception during first sex and less likely to receive formal sex education. (Guttmacher Institute, 2020)
Unplanned Pregnancy
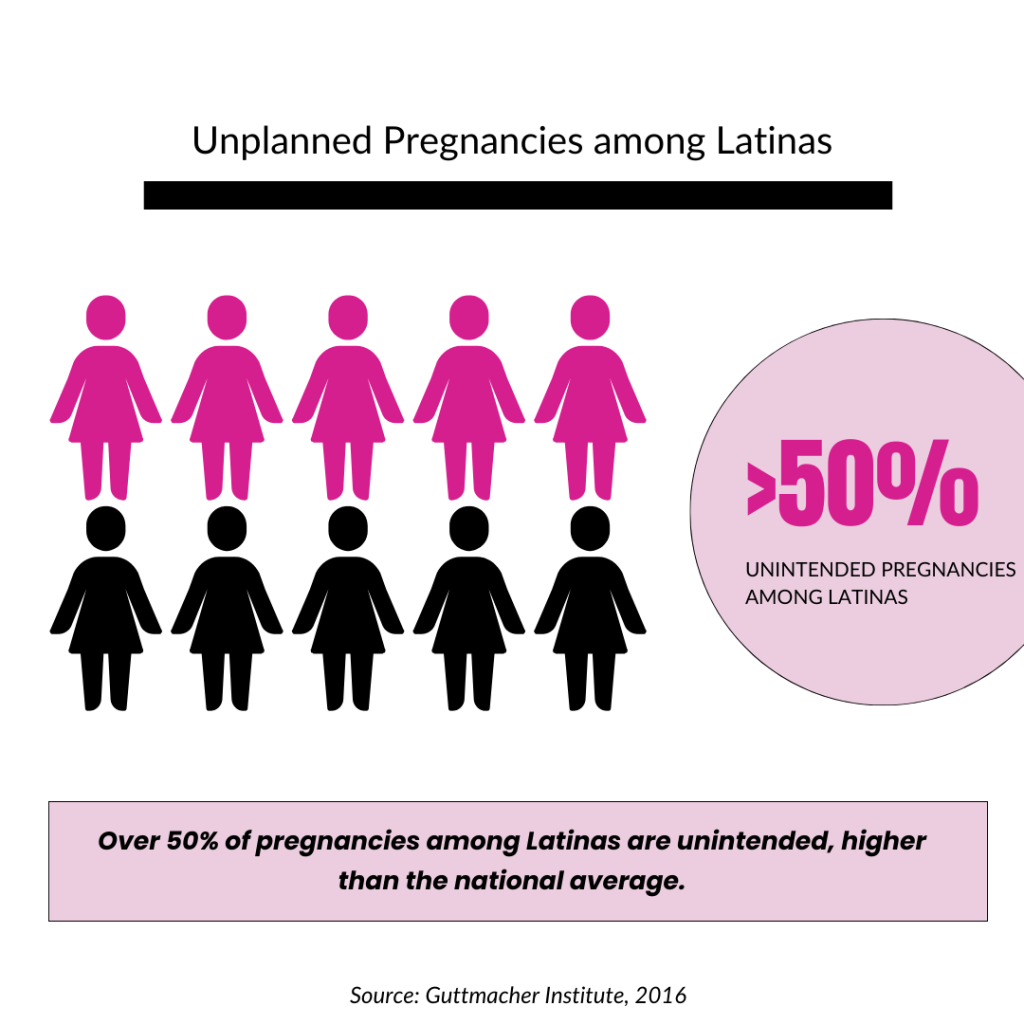
- Over 50% of pregnancies among Latinas are unintended, higher than the national average. (Guttmacher Institute, 2016)
- Unintended pregnancies are linked to delayed prenatal care, lower likelihood of breastfeeding, and poorer mental health outcomes—especially in communities with lower access to care. (CDC, 2023)
- Latinas are more likely to face barriers to contraception, including cost, lack of access, and immigration-related fears. (National Latina Institute for Reproductive Justice, 2021)
Programming, Policies & Recommendations
Current Policies
Note: These are existing policies we’ve compiled that are related to Sexual Health.
Federal Policies: These large-scale legislative frameworks influence access to sexual and reproductive health services for Latino communities.
Affordable Care Act (ACA)
Overview:
The Affordable Care Act (ACA) expanded access to healthcare through Medicaid expansion and the creation of insurance marketplaces. It also mandated coverage for many preventive services, including sexual health screenings.
Successes:
- Reduced Uninsured Rates: The ACA significantly reduced the uninsured rate among Latinos—from 32% in 2010 to 19% in 2016. KFF: Racial Equity and Health Policy, KFF: Health Coverage by Ethnicity
- Preventive Services Coverage: The ACA requires coverage of preventive services (e.g., HIV screening, STI testing, HPV vaccines) without cost-sharing, benefiting Latino populations. Healthcare.gov Preventive Services
Challenges:
- Medicaid Expansion Gaps: As of 2024, 10 states—many in the South—have not expanded Medicaid, disproportionately affecting low-income Latinos. KFF Medicaid Expansion Status
- Immigration Status Exclusions: Undocumented immigrants remain ineligible for ACA coverage, contributing to the Latino community’s high uninsured rate. KFF: Health Coverage for Immigrants
Title X Family Planning Program
Overview:
Title X provides federal funding for family planning services, including contraception, STI testing, and reproductive health education for low-income individuals.
Successes:
- Serving Underserved Communities: A significant portion of Title X patients are Latino, helping reduce access barriers to reproductive health and preventive services. HHS OPA Title X Facts
Challenges:
- Funding Cuts & Policy Restrictions: Between 2019 and 2021, funding cuts and policy changes led to a 63% reduction in Title X clinic sites, limiting access in many underserved Latino communities. Guttmacher Institute
Current Programs
National Programs: These federally funded or CDC-supported programs directly serve Latino communities and are shaped by the above policies.
Ryan White HIV/AIDS Program
Overview:
This federally funded program provides medical care, medications, and essential support services for people living with HIV, focusing on those who are uninsured or underinsured.
Successes:
- Improved HIV Care Access: In 2019, over half of Latinos diagnosed with HIV received services through the program, improving linkage to care and access to antiretroviral therapy.
HIV.gov Ryan White Data
Challenges:
- Disparities in Outcomes: While access has improved, racial and ethnic disparities in viral suppression persist, particularly among multiracial and Black Latino populations. HRSA 2020 RWHAP Annual Client-Level Data Report
CDC HIV/STI Education Campaigns & Interventions
Overview:
The CDC leads national campaigns and implements culturally tailored interventions to reduce HIV and STI rates in at-risk communities, including Latinos. These efforts promote education, testing, and prevention strategies such as condom use and PrEP.
Successes:
- Let’s Stop HIV Together: A national campaign aimed at raising awareness, reducing stigma, and promoting HIV testing and PrEP—particularly in communities of color, including Latinos. Visit campaign
- ¡Cuídate! : An evidence-based HIV/STI prevention curriculum designed for Latino adolescents. It emphasizes cultural values and personal responsibility and has been shown to increase condom use and improve HIV/STI knowledge. Learn more
Challenges:
- Language & Cultural Barriers: Despite these efforts, many Latino communities still face barriers due to limited bilingual outreach and cultural tailoring. Stigma surrounding sexual health topics in families can discourage open dialogue and engagement. Explore the Hispanic/Latino Toolkit
Policy and Programmatic Recommendations
Policy Recommendations:
Informed by Evidence: Policy Recommendations from Experts
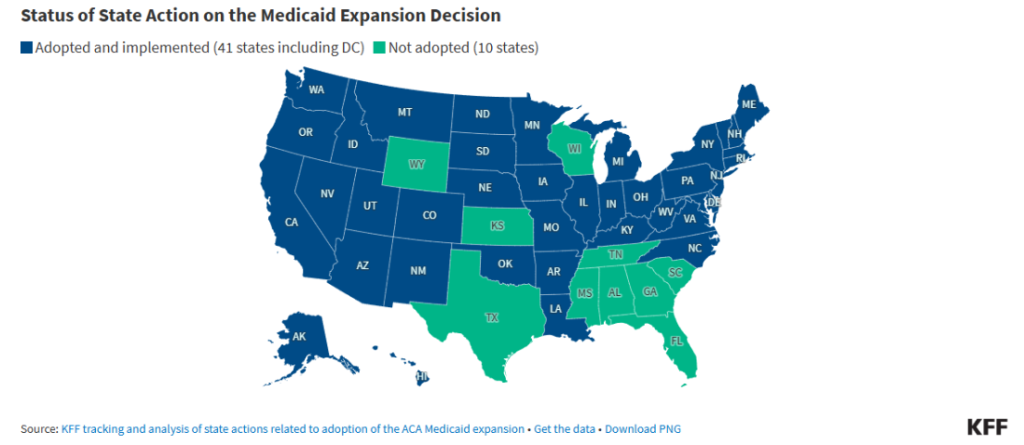
Expand Medicaid in States with Large Latino Populations
Many states that did not expand Medicaid under the ACA have significant Latino populations with unmet healthcare needs. More than half (55%) of the U.S. Hispanic population resides in three states: California, Florida, Texas. Some other states with large Latino populations include New York, Illinois, Arizona, New Jersey, and Colorado (Korhonen, 2024).
- Recommendation: Advocate for Medicaid expansion in states like Texas and Florida, where many low-income Latinos remain uninsured.
- Advocate for Medicaid expansion in states like Texas, Florida, and New York, where a large number of low-income Latinos remain uninsured.
- Advocacy Focus: Engage with local governments and healthcare providers to push for Medicaid expansion as a means to reduce sexual health disparities in Latino communities.
Evidence:
Increase Funding for the Ryan White HIV/AIDS Program
While the Ryan White program has been successful in helping Latinos with HIV, more resources are needed to close gaps in care for Black and multiracial Hispanic/Latino populations.
- Recommendation: Allocate targeted funding to reduce HIV disparities among Black and multiracial Hispanic/Latino individuals.
- Advocate for targeted funding within the Ryan White program to address disparities in viral suppression rates among Black and multiracial Hispanic/Latino individuals.
- Advocacy Focus: Push for state and federal policies that allocate additional resources to community health programs addressing HIV in minority groups.
Evidence:
Increase Funding for Title X Clinics in Latino Communities
Title X clinics are vital to providing affordable reproductive health services, but funding cuts have reduced their availability in some areas.
- Recommendation: Secure greater funding for Title X clinics in Latino-majority areas, especially those with high STI/HIV rates.
- Advocate for increased funding for Title X clinics in Latino-majority areas, particularly in states with high rates of STI and HIV infections. More funding will enable clinics to offer expanded services, such as comprehensive sexual health education, testing, and contraception.
- Advocacy Focus: Partner with reproductive justice organizations to campaign for greater state and federal funding for Title X programs.
Evidence:
Programmatic Recommendations
Service-oriented strategies implemented by healthcare systems, nonprofits, or local health departments.
Implement More Pop-Up Clinics in Latino Neighborhoods
Pop-up clinics can help provide convenient and affordable healthcare to underserved Latino communities.
- Recommendation: Expand mobile sexual health services in trusted community locations.
- Encourage healthcare systems and public health departments to set up more pop-up sexual health clinics in areas with high Latino populations. These clinics should offer bilingual services and partner with trusted community spaces like churches and schools to provide STI testing, contraception, and health education.
- Advocacy Focus: Secure funding through federal programs like Title X or local grants to support mobile health clinics in high-need areas.
Evidence:
Improve Outreach for Undocumented Latino Immigrants
Undocumented immigrants face significant barriers to accessing affordable healthcare.
- Recommendation: Create and expand programs offering low-cost or free sexual health care regardless of immigration status.
- Expand community health programs to specifically target undocumented immigrants for sexual health services, regardless of their insurance or immigration status. This includes providing access to free or low-cost HIV/STI testing, contraception, and health education.
- Advocacy Focus: Collaborate with non-profit organizations, such as the National Latina Institute for Reproductive Justice, to lobby for policies that provide undocumented individuals access to basic healthcare.
Evidence:
Enhance Cultural Competency in Sexual Health Campaigns
Many Latinos face cultural stigmas that prevent them from accessing sexual health services.
- Recommendation: Launch bilingual, stigma-reducing campaigns that reflect Latino cultural values.
- Design more culturally relevant sexual health campaigns, specifically targeting Latino families. These campaigns should address the cultural stigmas surrounding sexual health and be delivered in both Spanish and English, with a focus on reducing barriers to open discussion.
- Advocacy Focus: Work with Latino community leaders, healthcare providers, and media outlets to create and disseminate bilingual educational materials that promote sexual health services.
Evidence:

Invest in Peer Education & Promotores de Salud Models
Promotores de salud (community health workers) are trusted messengers in Latino communities. They help overcome barriers like stigma, fear, and low health literacy by providing culturally relevant, peer-led education and navigation support. Promotores have proven success in increasing HIV/STI testing and promoting healthy sexual behaviors.
- Recommendation: Encourage healthcare systems and public health departments to set up more pop-up sexual health clinics in areas with high Latino populations. These clinics should offer bilingual services and partner with trusted community spaces like churches and schools to provide STI testing, contraception, and health education.
- Expand investment in community-based peer educator programs that employ promotores to deliver bilingual, culturally relevant sexual health education and link individuals to services.
Evidence:
Expand Digital Health Interventions (Texts, Apps, Social Media)
Latinos, especially youth, have high mobile phone and social media use, but often lack access to traditional health services. Digital tools like apps and text reminders have been shown to improve HIV/STI prevention knowledge, increase condom use, and encourage clinic visits.
- Recommendation: Develop mobile-friendly bilingual platforms and use text-message or app-based reminders to promote STI testing, contraception use, and sexual health education.
Evidence:
Strengthen School-Based Health Education in Latino-Majority Districts
Many Latino adolescents attend schools that provide limited or abstinence-only sex education. These programs often lack cultural relevance and multilingual support, leaving youth underprepared to make informed decisions about sexual health.
- Recommendation: Support culturally responsive, bilingual sexual health education in schools that serve large Latino populations. Partner with school-based health centers to integrate STI testing and contraception access when possible.
Evidence:
Integrate Mental Health with Sexual Health Services
Latino youth, LGBTQ+ individuals, and those experiencing trauma face intersecting challenges in mental and sexual health. Poor mental health is associated with risky sexual behaviors and lower use of preventive services, yet mental and sexual health care are often siloed.
- Recommendation: Integrate trauma-informed, culturally competent mental health support within sexual health services—especially for vulnerable subgroups—either by co-locating services or through warm referrals.
Evidence:
Call to Action: Get Involved
The time to address sexual health inequities in the Latino community is now. We must collectively push for immediate and effective changes that support the sexual health and well-being of this population.
Take Action: Support Sexual Health Equity for Latino Communities

Speak up for inclusive, culturally responsive sexual health education and services. Here’s how you can help:
- Contact Your Decisionmakers: Urge them to support comprehensive, bilingual sex ed that includes topics like consent, contraception, and STI prevention — all taught with cultural respect.
→ Find Your State Lawmakers. - Support Policy Reform: Advocate for laws requiring schools to offer medically accurate, culturally relevant sex ed and for healthcare providers to be trained in cultural competence.
→ Sex Ed Policy by State – SIECUS - Join or Support Advocacy Groups: Get involved with organizations working to improve Latino sexual health education and access.
→ UnidosUS – Health Advocacy
→ Latino Commission on AIDS
→ Power to Decide
Together, we can break stigma, expand access, and create safer, healthier futures for Latino communities.
- Support Community Health Organizations: Donate to or volunteer with organizations that are focused on providing sexual health services to underserved Latino communities. These organizations play a critical role in bridging the gap in access to care.
- Raise Awareness: Use social media platforms and community forums to raise awareness of sexual health disparities in the Latino community. Share educational resources, promote bilingual services, and encourage conversations about sexual health without shame or stigma.
- Demand More Data and Research: Push for more comprehensive research on sexual health disparities within the Latino community, disaggregating data by factors such as race, sexual orientation, and economic status to inform more tailored interventions (Racial Differences in S…)(Martinez et al., 2017).
Through concerted efforts in policy, education, and community engagement, we can overcome the systemic barriers preventing Latinos from achieving sexual health equity. Together, we can ensure that every member of this community has access to the care and knowledge they deserve.
Partners and Resources for Families
🌍 Helpful Resources for Families
These groups offer direct services, education, and support for individuals and families:
Planned Parenthood
Description: Provides bilingual STI testing, contraception, and educational materials. Offers local clinics across the U.S. for easy access.
Website: plannedparenthood.org
Get care and services: Click here.
Info Pages: Click here.
Spanish: plannedparenthood.org/learn-es
Title X Family Planning Program
Description: Provides low-cost or free reproductive health services, including contraception and STI testing.
Adolescent Health: Click here.
Reproductive Health: Click here.
Find a Family Planning Clinic: Click here.

Bedsider (by Power to Decide)
Description: User-friendly info on birth control, sex, and health with tools like clinic finders and reminders.
Website: bedsider.org
Spanish: bedsider.org/es

2-1-1 – Information and Referral Services
Description: A free, confidential service available 24/7 to connect individuals with local community services, including food, housing, and disaster assistance.
Website: https://www.211.org/
Find your Local 2-1-1: Click here.
Additional Resources here:
- Latino Commission on AIDS
- Description: Offers HIV testing, community outreach, and culturally specific education programs for Latinos.
- Website: https://www.latinoaids.org
- National Latina Institute for Reproductive Justice
- Description: Offers bilingual resources and organizes grassroots advocacy centered on the reproductive rights of Latinas.
- Website: latinainstitute.org
- Ryan White HIV/AIDS Program
- Description: Supports low-income people living with HIV through healthcare, medications, and case management services.
- Website: hab.hrsa.gov
Teen & Youth Education
- Stay Teen – (Archived, but still helpful)
- Description: Teen-friendly explanations about relationships, consent, and decision-making.
Great for caregivers or programs working with teens. - Website: stayteen.org
- Description: Teen-friendly explanations about relationships, consent, and decision-making.
- Sex Positive Families –
- Description: A culturally affirming space for parents to get resources and tools to raise sexually healthy children. Offers a Free Resource Library.
- Website: sexpositivefamilies.com
HIV/PrEP Resources
- PleasePrEPMe –
- Description: Helps users find free or low-cost PrEP services and provides info in Spanish.
- Website: pleaseprepme.org
- HIV.gov – Spanish Resources –
- Description: Spanish language hub on HIV basics, testing, and prevention.
- Website: hiv.gov/espanol
Use these resources to support your families access to key sexual health education, information, and clinics.
🌍 Additional Resources and Data for Partners
These organizations are ideal for training, partnership, research, and system-level advocacy:
Helpful Resources for Health Information and Organizational Partners
National Hispanic Medical Association (NHMA)
👉 nhmamd.org
Focuses on training and supporting Latino health professionals and influencing health policy.
The Guttmacher Institute
👉 guttmacher.org
Provides research and data on sexual and reproductive health, useful for policy, program design, and advocacy.
Migrant Clinicians Network (MCN)
👉 migrantclinician.org
Supports frontline providers with mobile health delivery, training, and tools to serve migrant and underserved populations.
Cultural Competency & Latino Health
- Think Cultural Health (by HHS) – thinkculturalhealth.hhs.gov – https://thinkculturalhealth.hhs.gov/ Free CEU-accredited training for healthcare providers on cultural and linguistic competency.
- UnidosUS Health Policy Resources – unidosus.org– https://www.unidosus.org/resources/?topic=health
Reports and tools focused on Latino health equity and systemic barriers. - National Resource Center for Reaching Underserved Populations (NRCRUP) – reachingunderservedpopulations.org
Offers sexual health curricula and outreach materials for immigrant and refugee communities.
Program & Curriculum Tools
- SIECUS Sexuality Education Resources – siecus.org/resources Includes sex ed curricula guidance, policy updates, and best practices for community-level implementation.
- Advocates for Youth – advocatesforyouth.org
Offers curricula, trainings, and culturally relevant guides — e.g., the Rights, Respect, Responsibility curriculum is free and inclusive. - Guttmacher Institute Data Center – guttmacher.org/data-center Interactive data, state-level policies, and research on sexual and reproductive health.
Clinical Resources
National CLAS Standards (HHS) – thinkculturalhealth.hhs.gov/clas
Framework to guide health organizations in providing culturally and linguistically appropriate services.
CDC’s STD Treatment Guidelines – cdc.gov/std/treatment
The go-to resource for clinicians on STI diagnosis and treatment.
References
Click here to review all References:
| References |
| Advocates for Youth. (n.d.). Advocates for Youth resources. https://advocatesforyouth.org |
| Afable-Munsuz, A., et al. (2006). Latino teens are less likely to receive comprehensive sex ed, but benefit from culturally tailored programs. Retrieved from https://www.guttmacher.org/journals/psrh/2006/sexual-risk-taking-among-latina-adolescents-cultural-and-parental-influences |
| Afable-Munsuz, A., et al. (2006). Sexual risk-taking among Latina adolescents: The role of cultural and parental influences. Perspectives on Sexual and Reproductive Health. https://www.guttmacher.org/journals/psrh/2006/sexual-risk-taking-among-latina-adolescents-cultural-and-parental-influences |
| Arredondo, E. M., et al. (2013). Cultural values and condom use among Latino youth. Journal of Pediatric Psychology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3777941/ |
| Assistant Secretary for Planning and Evaluation (ASPE) Office of Health Policy. (2024). Health Insurance Coverage and Access to Care Among Latino Americans: Recent Trends and Key Challenges. https://aspe.hhs.gov/reports/health-insurance-coverage-access-care-latinos |
| Bureau, U. S. Census. (2024, September 16). Hispanic Heritage Month: 2024. https://www.census.gov/newsroom/facts-for-features/2024/hispanic-heritage-month.html |
| Calderon, M. (2021). Contraceptive access and experiences among Latina youth. Reproductive Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8141515/ |
| Castro, A. (2018). Promoting sexual health among Latinas. Journal of Women’s Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6002116/ |
| CDC. (2022). HIV surveillance data tables: Diagnoses, deaths, and prevalence of HIV in the united states and 6 territories and freely associated states tables, 2022. CDC Stacks. https://stacks.cdc.gov/view/cdc/156510 |
| CDC. (2024a, August 29). About AtlasPlus. National Center for HIV, Viral Hepatitis, STD, and Tuberculosis Prevention. https://www.cdc.gov/nchhstp/about/atlasplus.html |
| CDC. (2024b, October 2). Health disparities in Hispanic or Latino people. Health Disparities in HIV, Viral Hepatitis, STDs, & Tuberculosis. https://www.cdc.gov/health-disparities-hiv-std-tb-hepatitis/populations/hispanic-latino.html |
| Centers for Disease Control and Prevention. (2022). Births: Final data for 2021 (National Vital Statistics Reports, Vol. 72, No. 3). https://www.cdc.gov/nchs/data/nvsr/nvsr72/nvsr72-03.pdf |
| Centers for Disease Control and Prevention. (2022). HIV surveillance data tables: Diagnoses, deaths, and prevalence of HIV in the United States and 6 territories and freely associated states tables, 2022. https://stacks.cdc.gov/view/cdc/156510 |
| Centers for Disease Control and Prevention. (2023). Unintended pregnancy. U.S. Department of Health and Human Services. https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/index.htm |
| Centers for Disease Control and Prevention. (2024a, August 29). About AtlasPlus. https://www.cdc.gov/nchhstp/about/atlasplus.html |
| Centers for Disease Control and Prevention. (2024b, October 2). Health disparities in Hispanic or Latino people. https://www.cdc.gov/health-disparities-hiv-std-tb-hepatitis/populations/hispanic-latino.html |
| Centers for Disease Control and Prevention. (n.d.). Cuidate! Effective intervention program. https://www.cdc.gov/hiv/effective-interventions/prevent/educational/cuida-te/index.html |
| Centers for Disease Control and Prevention. (n.d.). STD treatment guidelines. https://www.cdc.gov/std/treatment |
| Courtemanche, C., et al. (2019). Impacts of the Affordable Care Act on reproductive health access. Health Affairs, 38(3), 482–490. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2019.00145 |
| Escobedo, L. E., Cervantes, L., & Havranek, E. (2023). Barriers in healthcare for Latinx patients with limited English proficiency: A narrative review. Journal of General Internal Medicine, 38(5), 1264–1271. https://doi.org/10.1007/s11606-022-07995-3 |
| García, J., et al. (2020). Barriers to health care among Latino gay men and transgender individuals. American Journal of Public Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7334369/ |
| Gómez, A. M., et al. (2019). Gender roles and reproductive health: Latino adolescents’ experiences. Journal of Adolescent Health. https://pubmed.ncbi.nlm.nih.gov/31282901/ |
| Guttmacher Institute. (2016). Unintended pregnancy in the United States. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states |
| Guttmacher Institute. (2020). Adolescents’ sexual and reproductive health. https://www.guttmacher.org/report/adolescents-sexual-and-reproductive-health-2020 |
| Guttmacher Institute. (2021). Title X under the Biden administration. https://www.guttmacher.org/article/2021/02/title-x-under-biden-administration-critical-moment-sexual-and-reproductive-health |
| Guttmacher Institute. (n.d.). Data center. https://www.guttmacher.org/data-center |
| Health Resources and Services Administration. (n.d.). Viral suppression data reports. https://hab.hrsa.gov/data/data-reports |
| Hill, L., Artiga, S., Damico, A., & Kaiser Family Foundation. (2024, January 11). Health coverage by race and ethnicity, 2010–2022. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/ |
| HIV.gov. (2024a). HIV statistics: Impact on racial and ethnic minorities. https://www.hiv.gov/hiv-basics/overview/data-and-trends/impact-on-racial-and-ethnic-minorities |
| HIV.gov. (2024b, August 15). HIV & AIDS trends and U.S. statistics overview. https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics |
| HIV.gov. (n.d.). Ryan White HIV/AIDS Program: Client demographics. https://www.hiv.gov/federal-response/ryan-white-hivaids-program/clients |
| Kaiser Family Foundation. (2024). U.S. HIV/AIDS snapshot. https://www.kff.org/hivaids/fact-sheet/u-s-hivaids-snapshot/ |
| Kaiser Family Foundation. (2024, October 15). The impact of HIV on Hispanic/Latino people in the United States. https://www.kff.org/hivaids/fact-sheet/the-impact-of-hiv-on-hispanic-latino-people-in-the-united-states/ |
| Kaiser Family Foundation. (n.d.). Health coverage and care of immigrants. https://www.kff.org/racial-equity-and-health-policy/fact-sheet/health-coverage-and-care-of-immigrants/ |
| Kaiser Family Foundation. (n.d.). Medicaid expansion decisions by state. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ |
| Korhonen, V. (2024). U.S. Hispanic population, by state 2023. Statista. https://www.statista.com/statistics/259850/hispanic-population-of-the-us-by-state/ |
| Lieberman, A. F., Ippen, C. G., & Van Horn, P. (2020). Latino youth benefit from culturally relevant, trauma-informed care. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32504151/ |
| Marin, B. V., et al. (2014). Acculturation and health behavior: The Latino paradox. Hispanic Journal of Behavioral Sciences. https://pubmed.ncbi.nlm.nih.gov/24590872/ |
| Martinez, O., Lee, J. H., Bandiera, F., Santamaria, E. K., Levine, E. C., & Operario, D. (2017). Sexual and behavioral health disparities among sexual minority Hispanics/Latinos: Findings from the National Health and Nutrition Examination Survey, 2001–2014. American Journal of Preventive Medicine, 53(2), 225–231. https://doi.org/10.1016/j.amepre.2017.01.037 |
| May, M., et al. (2012). Promotores improve health behaviors and trust in underserved Latino communities. Retrieved from https://www.researchgate.net/publication/235604656_Empowerment_of_Promotoras_as_Promotora-Researchers_in_the_Comidas_Saludables_Gente_Sana_en_las_Colonias_del_Sur_de_Tejas_Healthy_Food_and_Healthy_People_in_South_Texas_Colonias_Program |
| Morales-Alemán, M. M., & Scarinci, I. C. (2016). Correlates and predictors of sexual health among adolescent Latinas in the United States: A systematic review of the literature, 2004-2015. Preventive Medicine, 87, 183–193. https://doi.org/10.1016/j.ypmed.2016.03.005 |
| Morales-Alemán, M. M., Ferreti, G., & Scarinci, I. C. (2019). “I don’t like being stereotyped, I decided I was never going back to the doctor”: Sexual healthcare access among young Latina women in Alabama. Journal of Immigrant and Minority Health, 22(4), 645–652. https://doi.org/10.1007/s10903-019-00932-3 |
| Morales-Alemán, M. M., Scarinci, I. C., & McCallum, D. M. (2020). “It’s all about the children:” A participant-driven photo-elicitation study of Mexican and Puerto Rican Latina youth perceptions of sexual health and healthcare. International Journal of Environmental Research and Public Health, 17(6), 1967. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7078038/ |
| Muessig, K. E., et al. (2018). SMS interventions are effective in encouraging HIV/STI prevention behaviors. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6323863/ |
| Muñoz-Laboy, M., Severson, N., Martinez, O., et al. (2020). Community-based participatory research with Latino religious organizations: A case study. Journal of Religion and Health. https://pubmed.ncbi.nlm.nih.gov/32383910/ |
| National Latina Institute for Reproductive Justice. (2021). Abortion access. https://www.latinainstitute.org/en/issues/abortion-access |
| National Resource Center for Reaching Underserved Populations. (n.d.). https://reachingunderservedpopulations.org |
| Olayiwola, J. N., et al. (2023). Partnering with trusted spaces boosts community health engagement. Retrieved from https://www.mayoclinicproceedings.org/article/S0025-6196%2823%2900399-3/fulltext |
| Padilla, M., Luna-Gierke, R. E., Carree, T., Gutierrez, M., Yuan, X., & Dasgupta, S. (2023). Racial differences in social determinants of health and outcomes among Hispanic/Latino persons with HIV—United States, 2015–2020. Journal of Racial and Ethnic Health Disparities, 11(1), 574–588. https://doi.org/10.1007/s40615-023-01542-4 |
| Perez, M. (2011). Navigating sexuality education: Latina mothers’ perspectives. Sex Education. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3078981/ |
| Pirkis, J., Mok, K., & Williamson, M. (2024). Integrated care models improve outcomes in youth with overlapping mental and sexual health needs. Retrieved from https://journals.sagepub.com/doi/full/10.1177/00048674241256759 |
| Power to Decide. (2023). Teen pregnancy and race/ethnicity. https://powertodecide.org/what-we-do/information/teen-pregnancy/teen-pregnancy-and-race-ethnicity |
| PubMed. (2018). Economic burden of health disparities in the U.S., 2018. NIMHD. https://nimhd.nih.gov/about/publications/economic-burden-health-disparities-US-2018.html |
| Quality Interactions. (2020). Cultural and linguistic competency boosts patient trust and participation. Retrieved from https://www.qualityinteractions.com/blog/improving-patient-engagement-with-cultural-competency |
| Reiter, P. L., Pennell, M. L., Martinez, G. A., Perkins, R. B., & Katz, M. L. (2020). HPV vaccine coverage across Hispanic/Latinx subgroups in the United States. Cancer Causes & Control, 31(10), 905–914. https://doi.org/10.1007/s10552-020-01331-y |
| Rhodes, S. D., et al. (2017). Peer-led HIV/STI education increases testing and reduces transmission risk. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5570465/ |
| Rojas, P., et al. (2021). Addressing disparities in PrEP uptake: LGBTQ Latinx youth in the southern U.S. Journal of the International Association of Providers of AIDS Care. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7953734/ |
| Romero, D. (2020). Latinx health and PrEP access. AIDS and Behavior. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202220/ |
| Santelli, J. S., et al. (2022). Comprehensive sex education is linked to reduced STI rates and teen pregnancies. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8872707/ |
| Shokar, N. K., Doan, A., Calderon-Mora, J., et al. (2020). The prevalence of genital human papillomavirus subtypes in a cohort of Hispanic women presenting for cervical cancer screening along the US-Mexico border. Cancer Control, 27(1). https://doi.org/10.1177/1073274820951780 |
| SIECUS. (n.d.). Sexuality education resources. https://siecus.org/resources |
| Spencer, M. S., et al. (2017). Community Health Worker models are effective in Latino communities. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2623527 |
| Taylor, J. (2022). Racial equity in public health policy. Health Affairs Forefront. https://www.healthaffairs.org/do/10.1377/forefront.20220927.295304/ |
| U.S. Department of Health & Human Services Office of Minority Health Office of Minority Health. (2024). HIV/AIDS and Hispanic Americans. Office of Minority Health. https://minorityhealth.hhs.gov/hivaids-and-hispanic-americans |
| U.S. Department of Health & Human Services, Office of Population Affairs. (n.d.). Title X service grants. https://opa.hhs.gov/grant-programs/title-x-service-grants |
| U.S. Department of Health & Human Services. (n.d.). National CLAS Standards. https://thinkculturalhealth.hhs.gov/clas |
| U.S. Department of Health & Human Services. (n.d.). Think Cultural Health. https://thinkculturalhealth.hhs.gov |
| Wilson, E. K., et al. (2022). Mobile apps improve contraception use and sexual health literacy. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1054139X22006905 |
| Yu, S. W. Y., et al. (2020). Mobile clinics improve access to STI and preventive services. Retrieved from https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-020-1135-7 |
